Monday Poster Session
Category: Interventional Endoscopy
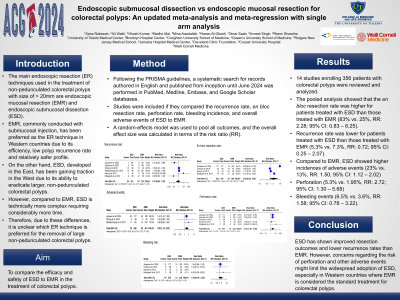
P2776 - Endoscopic Submucosal Dissection (ESD) vs Endoscopic Mucosal Resection (EMR) for Colorectal Polyps: An Updated Meta-Analysis and Meta-Regression With Single Arm Analysis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SR
Sana Rabeeah, MD
University of Toledo
Toledo, OH
Presenting Author(s)
Sana Rabeeah, MD1, Ali Wakil, MD2, Vikash Kumar, MD3, Madho Mal, MBBS4, Mina Awadallah, MD, MSc5, Hasan Al-Obaidi, MD6, Omar Saab, MD7, Avneet Singh, DO8, Reem Sharaiha, MD9
1University of Toledo, Toledo, OH; 2Brooklyn Hospital Center, Brooklyn, NY; 3Creighton University School of Medicine, Brooklyn, NY; 4Queen's University School of Medicine, Karachi, Sindh, Pakistan; 5Rutgers New Jersey Medical School, Newark, NJ; 6Jamaica Hospital Medical Center, Briarwood, NY; 7Cleveland Clinic Foundation, Westlake, OH; 8Cooper University Hospital, Camden, NJ; 9Weill Cornell Medicine, New York, NY
Introduction: Currently, the main endoscopic resection (ER) techniques used in the treatment of colorectal polyps are endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD). EMR, commonly conducted with submucosal injection, has been preferred as the ER technique for treating large, non-pedunculated colorectal polyps ≥20 mm in Western countries due to its efficiency, low recurrence rate and relatively safer profile. On the other hand, ESD, developed in the East, has been gaining interest from the West due to its ability to eradicate all large, non-pedunculated colorectal polyps. However, compared to EMR, ESD is more complex and requires considerably more time. Therefore, due to these differences, it is unclear which ER technique is preferred for the removal of colorectal polyps.
Methods: Following the PRISMA guidelines, a systematic search for records authored in English and published from inception until June 2024 was performed in PubMed, Medline, Embase, and Google Scholar databases. Studies were included if they compared the recurrence rate, en bloc resection rate, perforation rate, bleeding incidence, and overall adverse events of ESD to EMR. A random-effects model was used to pool all outcomes, and the overall effect size was calculated in terms of the risk ratio (RR).
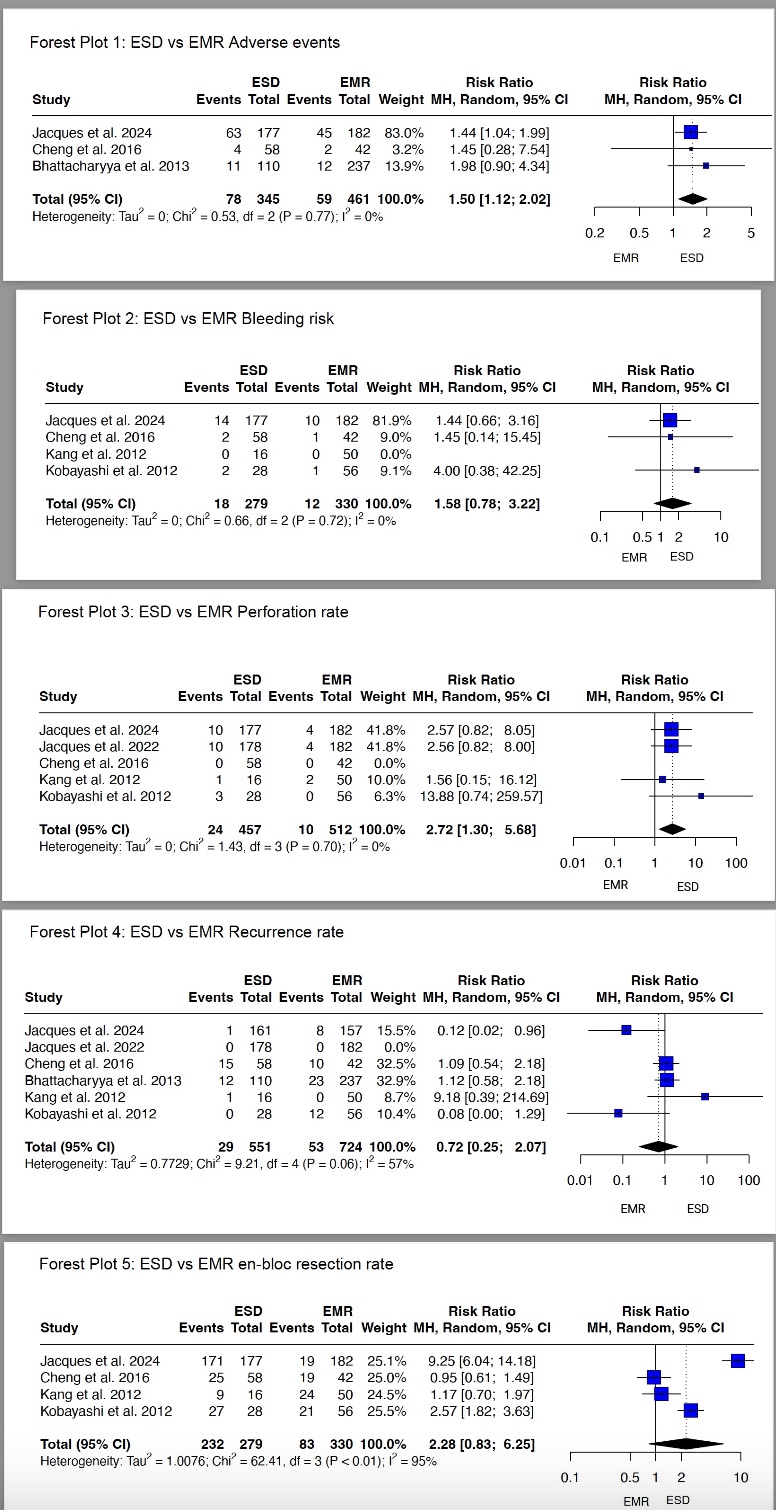
Results: 13 studies enrolling 356 patients with colorectal polyps were reviewed and analyzed. The pooled analysis showed that the en bloc resection rate was higher for patients treated with ESD than those treated with EMR (83% vs. 25%, RR: 2.28; 95% CI: 0.83 – 6.25). Furthermore, the recurrence rate was lower for patients treated with ESD than those treated with EMR (5.3% vs. 7.3%, RR: 0.72; 95% CI: 0.25 – 2.07). However, compared to EMR, ESD showed higher incidences of adverse events (23% vs. 13%, RR: 1.50; 95% CI: 1.12 – 2.02), perforation (5.3% vs. 1.95%, RR: 2.72; 95% CI: 1.30 – 5.68), and bleeding events (6.5% vs. 3.6%, RR: 1.58; 95% CI: 0.78 – 3.22).
Discussion: ESD has shown improved resection outcomes and lower recurrence rates than EMR. However, concerns regarding the risk of perforation and other adverse events might limit the widespread adoption of ESD for large polyps, especially in Western countries where EMR is considered the standard treatment for colorectal polyps.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sana Rabeeah, MD1, Ali Wakil, MD2, Vikash Kumar, MD3, Madho Mal, MBBS4, Mina Awadallah, MD, MSc5, Hasan Al-Obaidi, MD6, Omar Saab, MD7, Avneet Singh, DO8, Reem Sharaiha, MD9. P2776 - Endoscopic Submucosal Dissection (ESD) vs Endoscopic Mucosal Resection (EMR) for Colorectal Polyps: An Updated Meta-Analysis and Meta-Regression With Single Arm Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Toledo, Toledo, OH; 2Brooklyn Hospital Center, Brooklyn, NY; 3Creighton University School of Medicine, Brooklyn, NY; 4Queen's University School of Medicine, Karachi, Sindh, Pakistan; 5Rutgers New Jersey Medical School, Newark, NJ; 6Jamaica Hospital Medical Center, Briarwood, NY; 7Cleveland Clinic Foundation, Westlake, OH; 8Cooper University Hospital, Camden, NJ; 9Weill Cornell Medicine, New York, NY
Introduction: Currently, the main endoscopic resection (ER) techniques used in the treatment of colorectal polyps are endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD). EMR, commonly conducted with submucosal injection, has been preferred as the ER technique for treating large, non-pedunculated colorectal polyps ≥20 mm in Western countries due to its efficiency, low recurrence rate and relatively safer profile. On the other hand, ESD, developed in the East, has been gaining interest from the West due to its ability to eradicate all large, non-pedunculated colorectal polyps. However, compared to EMR, ESD is more complex and requires considerably more time. Therefore, due to these differences, it is unclear which ER technique is preferred for the removal of colorectal polyps.
Methods: Following the PRISMA guidelines, a systematic search for records authored in English and published from inception until June 2024 was performed in PubMed, Medline, Embase, and Google Scholar databases. Studies were included if they compared the recurrence rate, en bloc resection rate, perforation rate, bleeding incidence, and overall adverse events of ESD to EMR. A random-effects model was used to pool all outcomes, and the overall effect size was calculated in terms of the risk ratio (RR).
Results: 13 studies enrolling 356 patients with colorectal polyps were reviewed and analyzed. The pooled analysis showed that the en bloc resection rate was higher for patients treated with ESD than those treated with EMR (83% vs. 25%, RR: 2.28; 95% CI: 0.83 – 6.25). Furthermore, the recurrence rate was lower for patients treated with ESD than those treated with EMR (5.3% vs. 7.3%, RR: 0.72; 95% CI: 0.25 – 2.07). However, compared to EMR, ESD showed higher incidences of adverse events (23% vs. 13%, RR: 1.50; 95% CI: 1.12 – 2.02), perforation (5.3% vs. 1.95%, RR: 2.72; 95% CI: 1.30 – 5.68), and bleeding events (6.5% vs. 3.6%, RR: 1.58; 95% CI: 0.78 – 3.22).
Discussion: ESD has shown improved resection outcomes and lower recurrence rates than EMR. However, concerns regarding the risk of perforation and other adverse events might limit the widespread adoption of ESD for large polyps, especially in Western countries where EMR is considered the standard treatment for colorectal polyps.
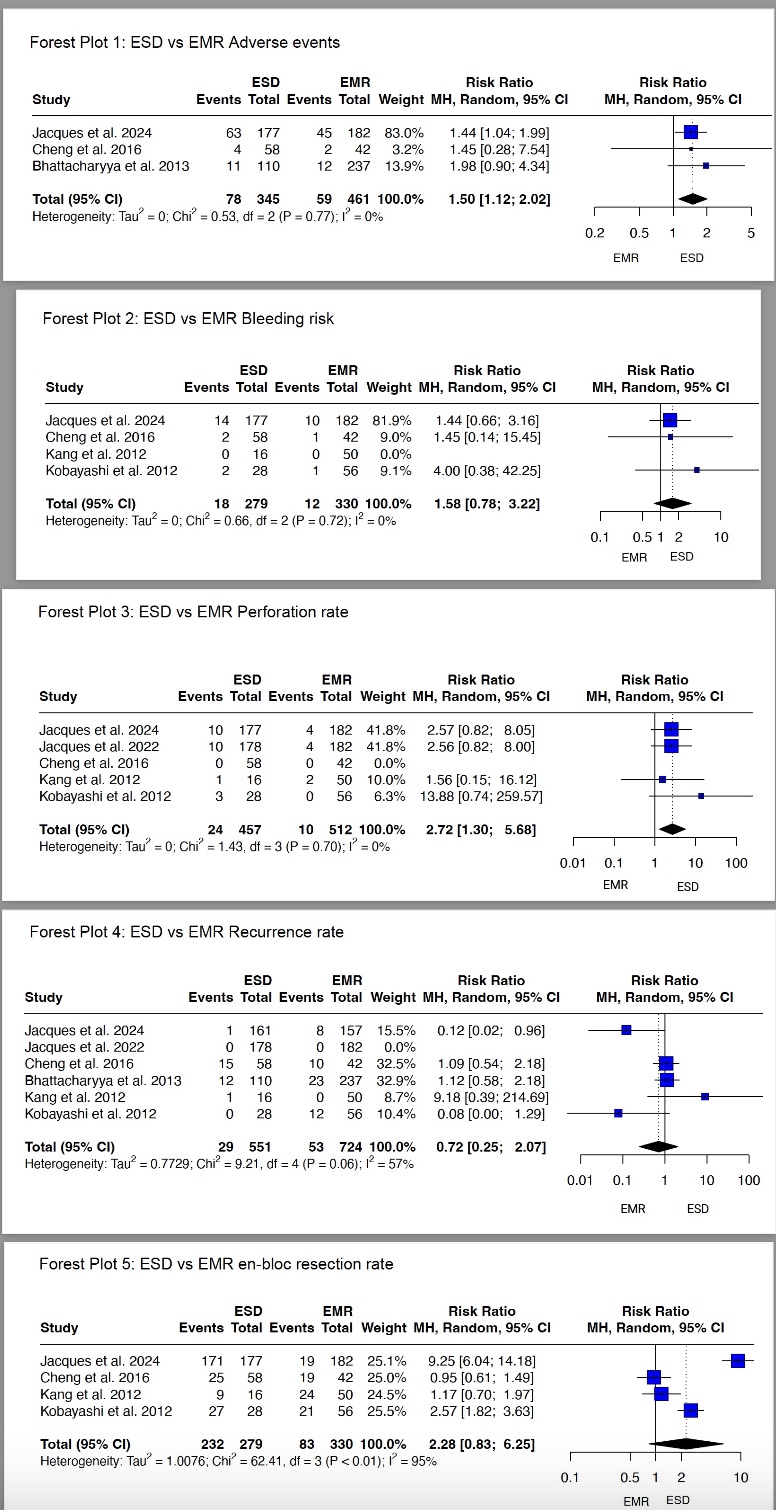
Figure: Forest Plots comparing ESD with EMR and their different outcomes
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sana Rabeeah indicated no relevant financial relationships.
Ali Wakil indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Madho Mal indicated no relevant financial relationships.
Mina Awadallah indicated no relevant financial relationships.
Hasan Al-Obaidi indicated no relevant financial relationships.
Omar Saab indicated no relevant financial relationships.
Avneet Singh indicated no relevant financial relationships.
Reem Sharaiha: Boston Scientific – Consultant, Grant/Research Support. Olympus – Consultant. Surgical Intuitive – Advisory Committee/Board Member.
Sana Rabeeah, MD1, Ali Wakil, MD2, Vikash Kumar, MD3, Madho Mal, MBBS4, Mina Awadallah, MD, MSc5, Hasan Al-Obaidi, MD6, Omar Saab, MD7, Avneet Singh, DO8, Reem Sharaiha, MD9. P2776 - Endoscopic Submucosal Dissection (ESD) vs Endoscopic Mucosal Resection (EMR) for Colorectal Polyps: An Updated Meta-Analysis and Meta-Regression With Single Arm Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
