Monday Poster Session
Category: Interventional Endoscopy
P2781 - Efficacy of Submucosal Injection in Endoscopic Papillectomy for Ampullary Tumors: A Meta-Analysis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Muhammad Shahzil, MD
Penn State Health Milton S. Hershey Medical Center
Hershey, PA
Presenting Author(s)
Muhammad Shahzil, MD1, Minahil Fatima, 2, Muhammad Saad Faisal, MD3, Maria Rehmani, 2, Ammad Javaid Chaudhry, MD3, Muhammad Ali Khaqan, MD4, Muhammad Salman Faisal, MD3
1Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 2King Edward Medical University, Lahore, Punjab, Pakistan; 3Henry Ford Health, Detroit, MI; 4John H. Stroger, Jr. Hospital of Cook County, Chicago, IL
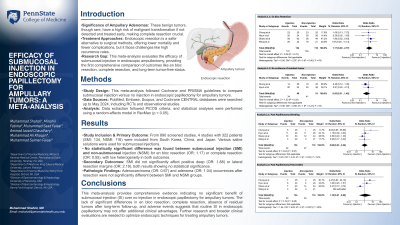
Introduction: Ampullary adenomas, originating from the ampulla of Vater (AoV), require complete resection due to their precancerous nature. Endoscopic papillectomy offers a less invasive alternative to surgery, but the use of submucosal injection (SI) in this procedure is not standardized, and its efficacy remains unclear due to the unique anatomy of the AoV. This meta-analysis evaluates the clinical efficacy of SI versus no injection before endoscopic papillectomy, focusing on complete resection rates and prevention of complications.
Methods: This meta-analysis followed Cochrane and PRISMA guidelines, comparing submucosal injection versus no injection in endoscopic papillectomy for ampullary tumors. We searched PubMed, Embase, Scopus, and Cochrane CENTRAL databases up to May 2024, including RCTs and observational studies. Data extraction followed PICOS criteria using Excel, and statistical analyses were performed with RevMan using a random-effects model (p < 0.05).
Results:
Discussion: This meta-analysis provides comprehensive evidence indicating no significant benefit of submucosal injection (SI) over no injection in endoscopic papillectomy for ampullary tumors. The lack of significant differences in en bloc resection, complete resection, absence of residual tumors after long-term follow-up, and adverse events suggests that routine SI in endoscopic papillectomy may not offer additional clinical advantages. Further research and broader clinical evaluations are needed to optimize endoscopic techniques for treating ampullary tumors.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Muhammad Shahzil, MD1, Minahil Fatima, 2, Muhammad Saad Faisal, MD3, Maria Rehmani, 2, Ammad Javaid Chaudhry, MD3, Muhammad Ali Khaqan, MD4, Muhammad Salman Faisal, MD3. P2781 - Efficacy of Submucosal Injection in Endoscopic Papillectomy for Ampullary Tumors: A Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 2King Edward Medical University, Lahore, Punjab, Pakistan; 3Henry Ford Health, Detroit, MI; 4John H. Stroger, Jr. Hospital of Cook County, Chicago, IL
Introduction: Ampullary adenomas, originating from the ampulla of Vater (AoV), require complete resection due to their precancerous nature. Endoscopic papillectomy offers a less invasive alternative to surgery, but the use of submucosal injection (SI) in this procedure is not standardized, and its efficacy remains unclear due to the unique anatomy of the AoV. This meta-analysis evaluates the clinical efficacy of SI versus no injection before endoscopic papillectomy, focusing on complete resection rates and prevention of complications.
Methods: This meta-analysis followed Cochrane and PRISMA guidelines, comparing submucosal injection versus no injection in endoscopic papillectomy for ampullary tumors. We searched PubMed, Embase, Scopus, and Cochrane CENTRAL databases up to May 2024, including RCTs and observational studies. Data extraction followed PICOS criteria using Excel, and statistical analyses were performed with RevMan using a random-effects model (p < 0.05).
Results:
Discussion: This meta-analysis provides comprehensive evidence indicating no significant benefit of submucosal injection (SI) over no injection in endoscopic papillectomy for ampullary tumors. The lack of significant differences in en bloc resection, complete resection, absence of residual tumors after long-term follow-up, and adverse events suggests that routine SI in endoscopic papillectomy may not offer additional clinical advantages. Further research and broader clinical evaluations are needed to optimize endoscopic techniques for treating ampullary tumors.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Muhammad Shahzil indicated no relevant financial relationships.
Minahil Fatima indicated no relevant financial relationships.
Muhammad Saad Faisal indicated no relevant financial relationships.
Maria Rehmani indicated no relevant financial relationships.
Ammad Javaid Chaudhry indicated no relevant financial relationships.
Muhammad Ali Khaqan indicated no relevant financial relationships.
Muhammad Salman Faisal indicated no relevant financial relationships.
Muhammad Shahzil, MD1, Minahil Fatima, 2, Muhammad Saad Faisal, MD3, Maria Rehmani, 2, Ammad Javaid Chaudhry, MD3, Muhammad Ali Khaqan, MD4, Muhammad Salman Faisal, MD3. P2781 - Efficacy of Submucosal Injection in Endoscopic Papillectomy for Ampullary Tumors: A Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
