Monday Poster Session
Category: Interventional Endoscopy
P2785 - A Systematic Review and Meta-Analysis on the Efficacy and Safety of Endoscopic Ultrasound Guided Radiofrequency Ablation in the Management of Patients With Pancreatic Malignancy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SK
Shahryar Khan, MD
University of Kansas
Overland Park, KS
Presenting Author(s)
Shahryar Khan, MD1, Amina Arif, MD2, Azzah Muhammad Hayat, MBBS3, Hoor Umar Afridi, MBBS4, Mashal Alam Khan, MBBS5, Yousaf Zafar, MD6
1University of Kansas, Overland Park, KS; 2University of Nevada, Reno School of Medicine, Peshawar, North-West Frontier, Pakistan; 3Khyber Medical University, Peshawar, North-West Frontier, Pakistan; 4Khyber Girls Medical College, Peshawar, North-West Frontier, Pakistan; 5Khyber Medical University, Overland Park, KS; 6University of Mississippi Medical Center, Madison, MS
Introduction: Pancreatic Malignancy (PM) is the second most common gastrointestinal malignancy with a poor prognosis. Surgery can provide long-term survival; however, most patients present with locally advanced cancer or metastasis which makes it unresectable. Endoscopic ultrasound guided Radiofrequency ablation (EUS-RFA) for Pancreatic Cystic Neoplasms (PCNs) and Neuroendocrine tumors (PNETs) have recently been used as a treatment modality for surgically inaccessible tumors with reportedly good clinical outcomes. A meticulous effort aimed at assessing the pooled safety and efficacy of EUS-RFA in PM was carried out in order to perform a systematic review and meta analysis.
Methods: PubMed and Embase were systematically searched to identify relevant studies published from inception through June 2024. The outcomes of interest were Clinical success (significant response more than 50% reduction in lesion diameter and/or equivalent development of a hypodense region (necrosis) on CT scan), Technical success (successful introduction of the needle within the target lesions with safe margins from the surrounding vital structures and application of RFA based on impedance), and Adverse Events (AEs). The random effects model was used to calculate the pooled mean effect (PME) with the corresponding 95% confidence intervals of our desired outcomes. Heterogeneity was assessed using the I2 Index. Data analysis was performed using MedCalc.
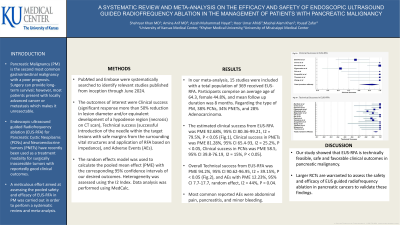
Results: In our meta-analysis, 15 studies were included with a total population of 369 received EUS-RFA. Participants comprise an average age of 64.3, female 44.8%, and mean follow up duration was 8 months. Regarding the type of PM, 38% PCNs, 34% PNETs, and 28% Adenocarcinoma. The estimated clinical success from EUS-RFA was PME 92.68%, 95% CI 80.36-99.21, I2 = 79.5%, P < 0.05 (Fig.1), Clinical success in PNETs was PME 81.28%, 95% CI 65.4-93, I2 = 25.2%, P < 0.05, Clinical success in PCNs was PME 58.5, 95% CI 39.8-76.19, I2 = 15%, P < 0.05, Overall Technical success from EUS-RFA was PME 94.2%, 95% CI 90.62-96.95, I2 = 39.15%, P < 0.05 (Fig.2), and AEs with PME 12.23%, 95% CI 7.7-17.7, random effect, I2 = 44%, P = 0.04. Most common reported AEs were abdominal pain, pancreatitis, and minor bleeding.
Discussion: Our study showed that EUS-RFA is technically feasible, safe and favorable clinical outcomes in pancreatic malignancy. Larger RCTs are warranted to assess the safety and efficacy of EUS guided radiofrequency ablation in pancreatic cancers to validate these findings.

Disclosures:
Shahryar Khan, MD1, Amina Arif, MD2, Azzah Muhammad Hayat, MBBS3, Hoor Umar Afridi, MBBS4, Mashal Alam Khan, MBBS5, Yousaf Zafar, MD6. P2785 - A Systematic Review and Meta-Analysis on the Efficacy and Safety of Endoscopic Ultrasound Guided Radiofrequency Ablation in the Management of Patients With Pancreatic Malignancy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Kansas, Overland Park, KS; 2University of Nevada, Reno School of Medicine, Peshawar, North-West Frontier, Pakistan; 3Khyber Medical University, Peshawar, North-West Frontier, Pakistan; 4Khyber Girls Medical College, Peshawar, North-West Frontier, Pakistan; 5Khyber Medical University, Overland Park, KS; 6University of Mississippi Medical Center, Madison, MS
Introduction: Pancreatic Malignancy (PM) is the second most common gastrointestinal malignancy with a poor prognosis. Surgery can provide long-term survival; however, most patients present with locally advanced cancer or metastasis which makes it unresectable. Endoscopic ultrasound guided Radiofrequency ablation (EUS-RFA) for Pancreatic Cystic Neoplasms (PCNs) and Neuroendocrine tumors (PNETs) have recently been used as a treatment modality for surgically inaccessible tumors with reportedly good clinical outcomes. A meticulous effort aimed at assessing the pooled safety and efficacy of EUS-RFA in PM was carried out in order to perform a systematic review and meta analysis.
Methods: PubMed and Embase were systematically searched to identify relevant studies published from inception through June 2024. The outcomes of interest were Clinical success (significant response more than 50% reduction in lesion diameter and/or equivalent development of a hypodense region (necrosis) on CT scan), Technical success (successful introduction of the needle within the target lesions with safe margins from the surrounding vital structures and application of RFA based on impedance), and Adverse Events (AEs). The random effects model was used to calculate the pooled mean effect (PME) with the corresponding 95% confidence intervals of our desired outcomes. Heterogeneity was assessed using the I2 Index. Data analysis was performed using MedCalc.
Results: In our meta-analysis, 15 studies were included with a total population of 369 received EUS-RFA. Participants comprise an average age of 64.3, female 44.8%, and mean follow up duration was 8 months. Regarding the type of PM, 38% PCNs, 34% PNETs, and 28% Adenocarcinoma. The estimated clinical success from EUS-RFA was PME 92.68%, 95% CI 80.36-99.21, I2 = 79.5%, P < 0.05 (Fig.1), Clinical success in PNETs was PME 81.28%, 95% CI 65.4-93, I2 = 25.2%, P < 0.05, Clinical success in PCNs was PME 58.5, 95% CI 39.8-76.19, I2 = 15%, P < 0.05, Overall Technical success from EUS-RFA was PME 94.2%, 95% CI 90.62-96.95, I2 = 39.15%, P < 0.05 (Fig.2), and AEs with PME 12.23%, 95% CI 7.7-17.7, random effect, I2 = 44%, P = 0.04. Most common reported AEs were abdominal pain, pancreatitis, and minor bleeding.
Discussion: Our study showed that EUS-RFA is technically feasible, safe and favorable clinical outcomes in pancreatic malignancy. Larger RCTs are warranted to assess the safety and efficacy of EUS guided radiofrequency ablation in pancreatic cancers to validate these findings.

Figure: Forrest Plots of Clinical Success and Technical Success in EUS-RFA
Disclosures:
Shahryar Khan indicated no relevant financial relationships.
Amina Arif indicated no relevant financial relationships.
Azzah Muhammad Hayat indicated no relevant financial relationships.
Hoor Umar Afridi indicated no relevant financial relationships.
Mashal Alam Khan indicated no relevant financial relationships.
Yousaf Zafar indicated no relevant financial relationships.
Shahryar Khan, MD1, Amina Arif, MD2, Azzah Muhammad Hayat, MBBS3, Hoor Umar Afridi, MBBS4, Mashal Alam Khan, MBBS5, Yousaf Zafar, MD6. P2785 - A Systematic Review and Meta-Analysis on the Efficacy and Safety of Endoscopic Ultrasound Guided Radiofrequency Ablation in the Management of Patients With Pancreatic Malignancy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
