Monday Poster Session
Category: Interventional Endoscopy
P2787 - Poorly Cohesive Subtype of Gastro-Esophageal Cancers Impacts Endoscopic Ultrasound Tumor Stage
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Andrew Alabd, MD
Cooper University Health Care
Camden, NJ
Presenting Author(s)
Andrew Alabd, MD1, Margaret Park, PhD2, Aamir Dam, MD2, Anjuli Luthra, MD2, Saraswathi Cappelle, MD2, Luis Pena, MD2, Andrew Sinnamon, MD2, Jose Pimiento, MD2, Mark Friedman, MD2, Rutika Mehta, MD2, Gregory Lauwers, MD2, Jennifer Permuth, PhD2, Shaffer Mok, MD2
1Cooper University Health Care, Camden, NJ; 2Moffitt Cancer Center, Tampa, FL
Introduction: Accurate locoregional cancer staging is essential for determining the prognosis and selecting the appropriate treatment in gastroesophageal cancer (GEC). This study aims to compare the initial EUS T staging with the final pathological staging in poorly cohesive cell types (PC) versus non-poorly cohesive (NPC) subtypes.
Methods: In this IRB-approved study, demographics, EUS staging, and pathological staging data were collected from 4,426 patients with GEC. We subdivided patients based on whether they received NAT and analyzed stage concordance and discordance in relation to histology. Chi-square analysis of independence was performed to assess the relationship between histology and stage concordance.
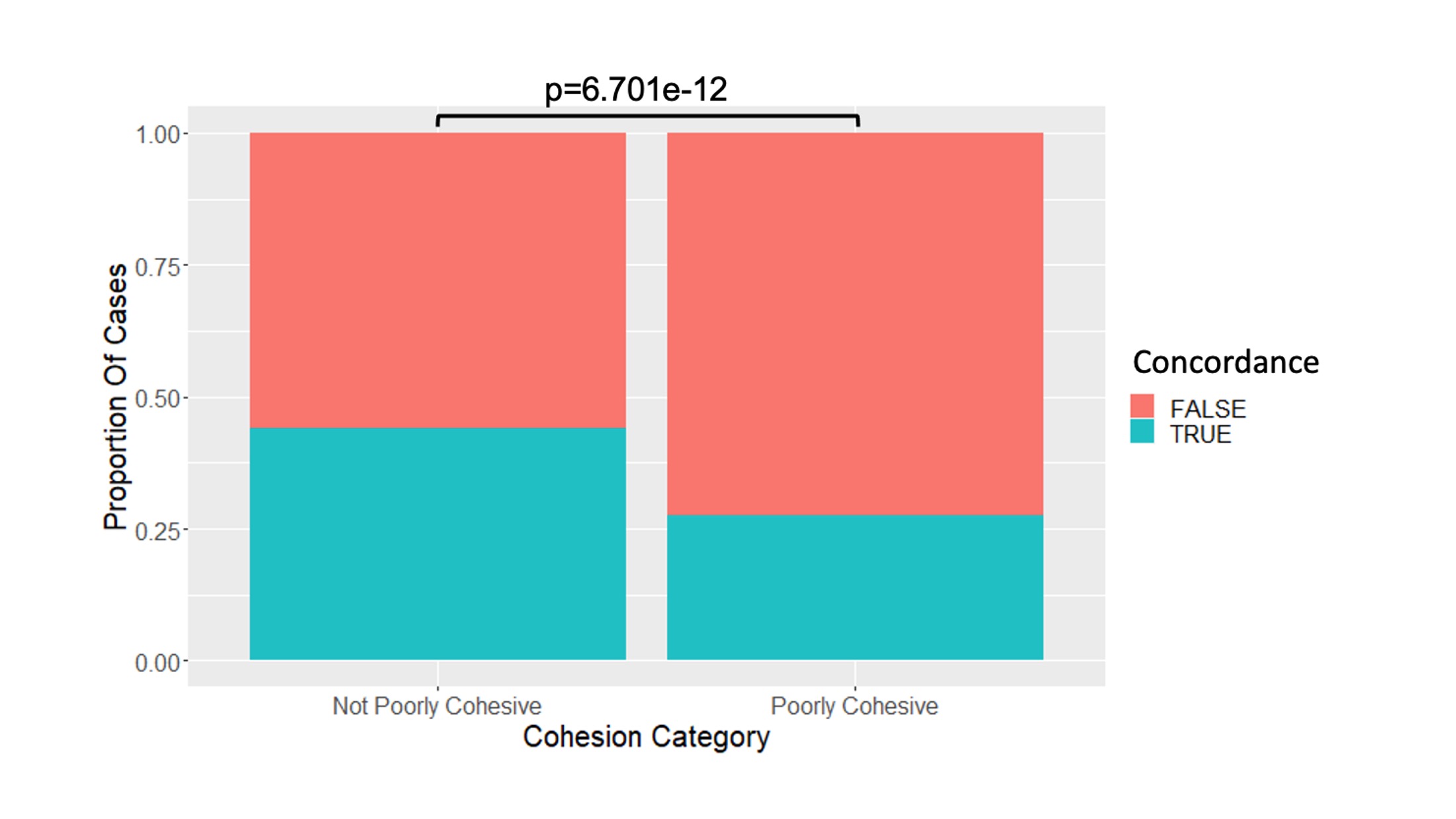
Results: We compared the initial EUS T staging to the final pathological staging in PC versus NPC GEC subtypes. There was a predominance of non-Hispanic white patients in the cohort. The results showed a higher frequency of males (77.5%). Most patients had NPC (89.3%), with 60.9% showing discordance between EUS and pathological staging. For all gastric and esophageal patients who did not receive NAT, Group 1 (n=2,344), EUS T stage showed concordance with the final pathology staging in 27.7% of PC histology cases versus 43.4% for NPC histology (p=0.001) (Figure 1). When evaluating PC versus NPC in only gastric cancer primary sites, the differences in concordance remained significant (p=0.001).
Discussion: Regardless of NAT status, T stage was more discordant in PC compared to NPC histologic subtypes. This difference persisted for GEC and gastric cancer but not for esophageal cancer. Strengths of this study include the large sample size, the complexity of the data, and the implications for various clinical practice environments. However, potential limitations include the inability to evaluate distant metastases (M stage), which could impact disease status. The cohort's predominance of non-Hispanic white males may limit generalizability. When comparing EUS versus final histopathologic stages in PC versus NPC GECs, we found a significant difference in stage concordance, with NPC showing higher concordance than PC. This difference persisted regardless of NAT administration. Given the histologic and endoscopic characteristics of PC, EUS T staging should be approached with caution when determining subsequent cancer care steps for these patients. Future studies evaluating EUS T stage in cohorts with known or unknown histology at the time of EUS may be valuable.
Disclosures:
Andrew Alabd, MD1, Margaret Park, PhD2, Aamir Dam, MD2, Anjuli Luthra, MD2, Saraswathi Cappelle, MD2, Luis Pena, MD2, Andrew Sinnamon, MD2, Jose Pimiento, MD2, Mark Friedman, MD2, Rutika Mehta, MD2, Gregory Lauwers, MD2, Jennifer Permuth, PhD2, Shaffer Mok, MD2. P2787 - Poorly Cohesive Subtype of Gastro-Esophageal Cancers Impacts Endoscopic Ultrasound Tumor Stage, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cooper University Health Care, Camden, NJ; 2Moffitt Cancer Center, Tampa, FL
Introduction: Accurate locoregional cancer staging is essential for determining the prognosis and selecting the appropriate treatment in gastroesophageal cancer (GEC). This study aims to compare the initial EUS T staging with the final pathological staging in poorly cohesive cell types (PC) versus non-poorly cohesive (NPC) subtypes.
Methods: In this IRB-approved study, demographics, EUS staging, and pathological staging data were collected from 4,426 patients with GEC. We subdivided patients based on whether they received NAT and analyzed stage concordance and discordance in relation to histology. Chi-square analysis of independence was performed to assess the relationship between histology and stage concordance.
Results: We compared the initial EUS T staging to the final pathological staging in PC versus NPC GEC subtypes. There was a predominance of non-Hispanic white patients in the cohort. The results showed a higher frequency of males (77.5%). Most patients had NPC (89.3%), with 60.9% showing discordance between EUS and pathological staging. For all gastric and esophageal patients who did not receive NAT, Group 1 (n=2,344), EUS T stage showed concordance with the final pathology staging in 27.7% of PC histology cases versus 43.4% for NPC histology (p=0.001) (Figure 1). When evaluating PC versus NPC in only gastric cancer primary sites, the differences in concordance remained significant (p=0.001).
Discussion: Regardless of NAT status, T stage was more discordant in PC compared to NPC histologic subtypes. This difference persisted for GEC and gastric cancer but not for esophageal cancer. Strengths of this study include the large sample size, the complexity of the data, and the implications for various clinical practice environments. However, potential limitations include the inability to evaluate distant metastases (M stage), which could impact disease status. The cohort's predominance of non-Hispanic white males may limit generalizability. When comparing EUS versus final histopathologic stages in PC versus NPC GECs, we found a significant difference in stage concordance, with NPC showing higher concordance than PC. This difference persisted regardless of NAT administration. Given the histologic and endoscopic characteristics of PC, EUS T staging should be approached with caution when determining subsequent cancer care steps for these patients. Future studies evaluating EUS T stage in cohorts with known or unknown histology at the time of EUS may be valuable.
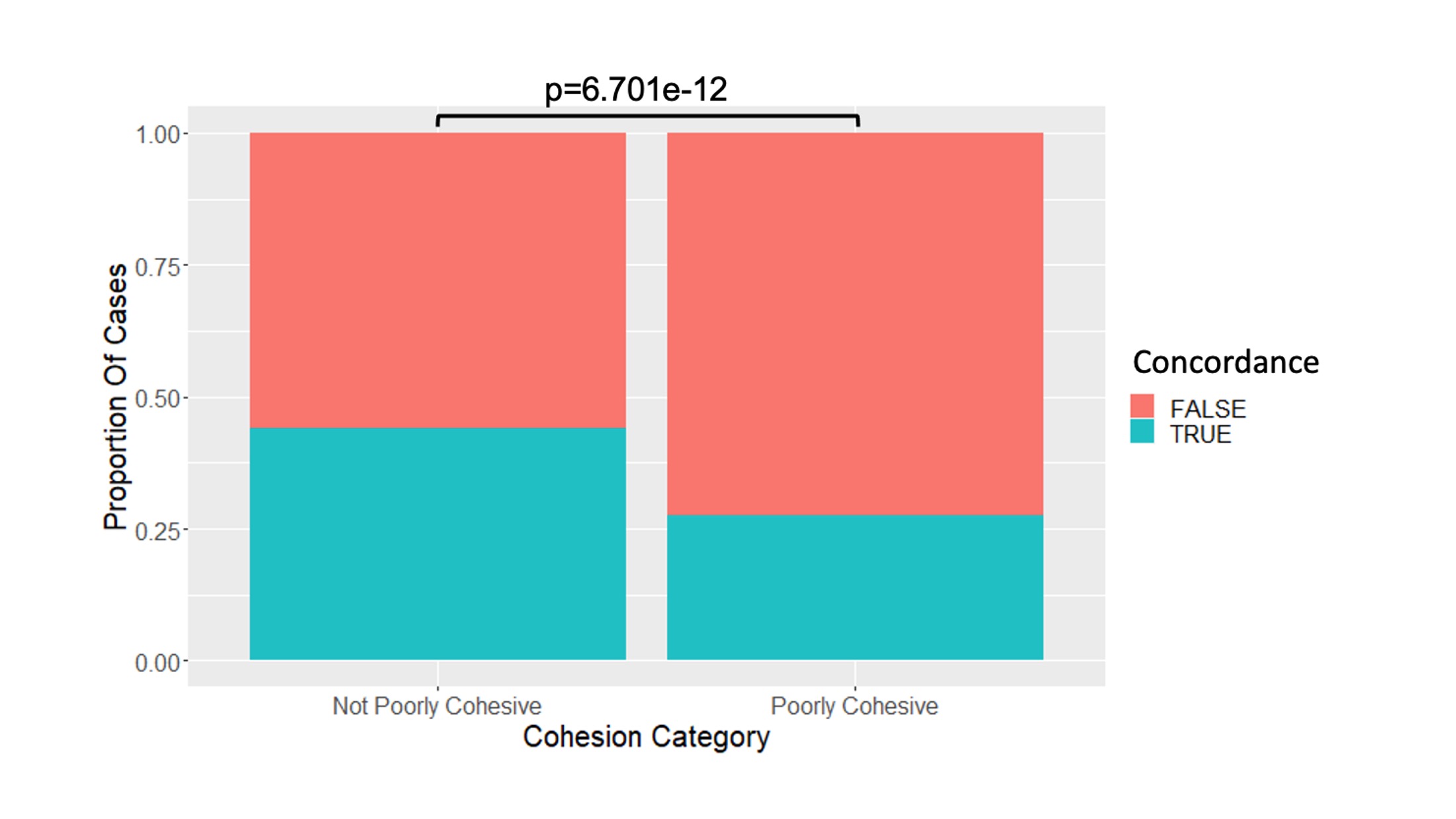
Figure: Figure 1: EUS Stage Concordance in poorly cohesive versus non-poorly cohesive GEC patients
Disclosures:
Andrew Alabd indicated no relevant financial relationships.
Margaret Park indicated no relevant financial relationships.
Aamir Dam indicated no relevant financial relationships.
Anjuli Luthra indicated no relevant financial relationships.
Saraswathi Cappelle indicated no relevant financial relationships.
Luis Pena indicated no relevant financial relationships.
Andrew Sinnamon indicated no relevant financial relationships.
Jose Pimiento indicated no relevant financial relationships.
Mark Friedman indicated no relevant financial relationships.
Rutika Mehta indicated no relevant financial relationships.
Gregory Lauwers indicated no relevant financial relationships.
Jennifer Permuth indicated no relevant financial relationships.
Shaffer Mok: C2/Pentax – Consultant. Steris – Consultant.
Andrew Alabd, MD1, Margaret Park, PhD2, Aamir Dam, MD2, Anjuli Luthra, MD2, Saraswathi Cappelle, MD2, Luis Pena, MD2, Andrew Sinnamon, MD2, Jose Pimiento, MD2, Mark Friedman, MD2, Rutika Mehta, MD2, Gregory Lauwers, MD2, Jennifer Permuth, PhD2, Shaffer Mok, MD2. P2787 - Poorly Cohesive Subtype of Gastro-Esophageal Cancers Impacts Endoscopic Ultrasound Tumor Stage, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
