Monday Poster Session
Category: IBD
P2694 - The Proof is in the Pathology: Fistulizing Endometriosis as a Rare Mimic of IBD
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Preethi Venkat, MD
University of Virginia Medical Center
Charlottesville, VA
Presenting Author(s)
Preethi Venkat, MD1, Hannah Laird, MD1, Olivia Becker, MD2, Amy Doran, MD2
1University of Virginia Medical Center, Charlottesville, VA; 2University of Virginia, Charlottesville, VA
Introduction: Various conditions can mimic inflammatory bowel disease (IBD) due to symptom overlap or imaging findings, resulting in potential delays in diagnosis.
We report a case of a patient with endometriosis and recurrent small bowel obstruction (SBO) with imaging evidence of small bowel stricture and fistulae. These findings, initially concerning for underlying Crohn’s disease, were later attributed to advanced endometriosis following histologic confirmation.
Case Description/Methods: A 41-year-old woman with a history of prior cesarean section, two hernia repairs, endometriosis status post diagnostic laparoscopy with excision, and recurrent SBO thought secondary to adhesions presented to the hospital with acute on chronic abdominal pain, nausea, and vomiting. She had two prior colonoscopies for SBO workup, which both demonstrated a prominent appendiceal orifice and normal terminal ileum (TI) biopsies. On admission, abdominopelvic computed tomography (CT) demonstrated SBO with a transition point at the level of a small bowel stricture at the terminal ileum, three regions of narrowing within the distal ileum, a sinus tract arising from the TI, and a possible right perianal sinus tract. Her labs were notable for a mildly elevated c-reactive protein and fecal calprotectin. Gastroenterology was consulted due to concern for Crohn’s disease. The SBO was initially managed conservatively with nasogastric tube (NGT) decompression. Though there was significant concern for Crohn's disease, repeat endoscopy was deferred in the setting of SBO. She began having regular bowel movements but continued to have high output from NGT, prompting surgical intervention with ileocecal resection. The pathology findings of the resected small bowel were consistent with endometriosis involving the bowel wall.
Discussion: Endometriosis frequently presents with GI symptoms, with the bowel representing 4-37% of endometriosis involvement outside the genital tract. Rarely, endometriosis can also cause abscesses or fistulae that mimic penetrating Crohn’s disease.1 This case highlights the overlap between IBD and endometriosis and the importance of keeping advanced endometriosis on the differential for young, menstruating women presenting with abdominal complaints or obstructive symptoms.
1. Foulon et al. Bowel Endometriosis Mimicking Crohn Disease. Inflammatory Bowel Diseases. 2021;27(3):e26-e27.

Disclosures:
Preethi Venkat, MD1, Hannah Laird, MD1, Olivia Becker, MD2, Amy Doran, MD2. P2694 - The Proof is in the Pathology: Fistulizing Endometriosis as a Rare Mimic of IBD, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Virginia Medical Center, Charlottesville, VA; 2University of Virginia, Charlottesville, VA
Introduction: Various conditions can mimic inflammatory bowel disease (IBD) due to symptom overlap or imaging findings, resulting in potential delays in diagnosis.
We report a case of a patient with endometriosis and recurrent small bowel obstruction (SBO) with imaging evidence of small bowel stricture and fistulae. These findings, initially concerning for underlying Crohn’s disease, were later attributed to advanced endometriosis following histologic confirmation.
Case Description/Methods: A 41-year-old woman with a history of prior cesarean section, two hernia repairs, endometriosis status post diagnostic laparoscopy with excision, and recurrent SBO thought secondary to adhesions presented to the hospital with acute on chronic abdominal pain, nausea, and vomiting. She had two prior colonoscopies for SBO workup, which both demonstrated a prominent appendiceal orifice and normal terminal ileum (TI) biopsies. On admission, abdominopelvic computed tomography (CT) demonstrated SBO with a transition point at the level of a small bowel stricture at the terminal ileum, three regions of narrowing within the distal ileum, a sinus tract arising from the TI, and a possible right perianal sinus tract. Her labs were notable for a mildly elevated c-reactive protein and fecal calprotectin. Gastroenterology was consulted due to concern for Crohn’s disease. The SBO was initially managed conservatively with nasogastric tube (NGT) decompression. Though there was significant concern for Crohn's disease, repeat endoscopy was deferred in the setting of SBO. She began having regular bowel movements but continued to have high output from NGT, prompting surgical intervention with ileocecal resection. The pathology findings of the resected small bowel were consistent with endometriosis involving the bowel wall.
Discussion: Endometriosis frequently presents with GI symptoms, with the bowel representing 4-37% of endometriosis involvement outside the genital tract. Rarely, endometriosis can also cause abscesses or fistulae that mimic penetrating Crohn’s disease.1 This case highlights the overlap between IBD and endometriosis and the importance of keeping advanced endometriosis on the differential for young, menstruating women presenting with abdominal complaints or obstructive symptoms.
1. Foulon et al. Bowel Endometriosis Mimicking Crohn Disease. Inflammatory Bowel Diseases. 2021;27(3):e26-e27.

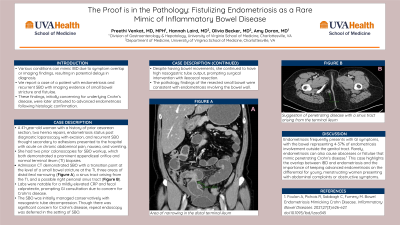
Figure: (A) Area of narrowing in the distal terminal ileum and (B) Suggestion of penetrating disease with a sinus tract arising from the terminal ileum.
Disclosures:
Preethi Venkat indicated no relevant financial relationships.
Hannah Laird indicated no relevant financial relationships.
Olivia Becker indicated no relevant financial relationships.
Amy Doran indicated no relevant financial relationships.
Preethi Venkat, MD1, Hannah Laird, MD1, Olivia Becker, MD2, Amy Doran, MD2. P2694 - The Proof is in the Pathology: Fistulizing Endometriosis as a Rare Mimic of IBD, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
