Monday Poster Session
Category: IBD
P2701 - A Rare Case of Immune Thrombocytopenic Purpura in the Setting of Ulcerative Colitis and Cytomegalovirus
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Niraj Shah, BS
Rowan-Virtua School of Osteopathic Medicine
Lawnside, NJ
Presenting Author(s)
Niraj Shah, BS1, Sanket Patel, DO2
1Rowan-Virtua School of Osteopathic Medicine, Lawnside, NJ; 2Virtua Health System, Moorestown, NJ
Introduction: Immune thrombocytopenic purpura (ITP) is an acquired thrombocytopenia with a rare association with inflammatory bowel disease (IBD). It is poorly understood and may be related to possible antigen cross-reactivity. It may also be triggered by infections like cytomegalovirus (CMV). We present a unique case of a patient with ulcerative colitis (UC) who developed concomitant ITP and CMV viremia.
Case Description/Methods: A 72-year-old woman with UC, hip replacement, hypertension, and treatment history of mesalamine non-response, azathioprine intolerance, vedolizumab non-response, and adalimumab immunogenic failure presented with worsening hematochezia and epistaxis. She was recently hospitalized for an IBD flare at a local hospital with platelet decline from 150,000 to 44,000 during admission which improved on high-dose steroids. She was also noted to have Bacteroides fragilis bacteremia successfully treated with antibiotics.
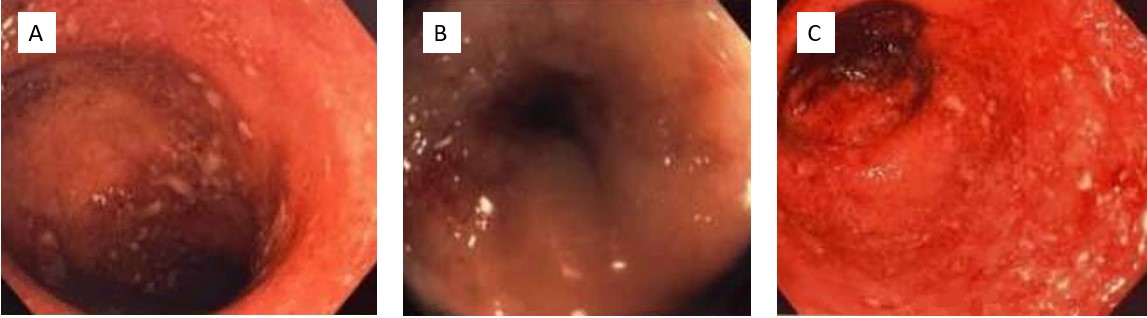
On readmission, vitals were stable, and she appeared nontoxic. Labs showed Hgb 8.2 g/dL, platelets 2*10^3/µL, CRP 3.2, and albumin 2.8. CT revealed pancolitis. Sigmoidoscopy showed Mayo 3 disease and rectosigmoid narrowing (Figure 1). She was treated with high-dose steroids and IVIG for recurrent ITP. CMV viremia (PCR 20,611 IU/mL) with indeterminate colonic biopsy was noted. She responded to foscarnet and was discharged on valganciclovir, prolonged prednisone taper, and prophylactic trimethoprim-sulfamethoxazole.
Follow-up in the IBD clinic included infliximab (10 mg/kg) monotherapy induction with shared-decision making and a notable improvement in CRP, but she developed serum sickness-like reaction after two induction doses with undetectable antibodies and a week 2 level of 35 µg/mL. A DVT in her left lower extremity led to apixaban initiation. Limited steroid response led to upadacitinib initiation with clinical response and without ITP recurrence.
Discussion: ITP may develop from untreated or active UC via molecular mimicry but can also be triggered by infections. This case highlights ITP recurrence probably due to refractory UC and exacerbated by opportunistic CMV. A heightened index of suspicion is warranted to look for infections in the context of a flaring IBD patient with thrombocytopenia. Further research is needed to understand the interaction between UC and ITP to optimize management and understand infection interplay in these clinical scenarios.
Disclosures:
Niraj Shah, BS1, Sanket Patel, DO2. P2701 - A Rare Case of Immune Thrombocytopenic Purpura in the Setting of Ulcerative Colitis and Cytomegalovirus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Rowan-Virtua School of Osteopathic Medicine, Lawnside, NJ; 2Virtua Health System, Moorestown, NJ
Introduction: Immune thrombocytopenic purpura (ITP) is an acquired thrombocytopenia with a rare association with inflammatory bowel disease (IBD). It is poorly understood and may be related to possible antigen cross-reactivity. It may also be triggered by infections like cytomegalovirus (CMV). We present a unique case of a patient with ulcerative colitis (UC) who developed concomitant ITP and CMV viremia.
Case Description/Methods: A 72-year-old woman with UC, hip replacement, hypertension, and treatment history of mesalamine non-response, azathioprine intolerance, vedolizumab non-response, and adalimumab immunogenic failure presented with worsening hematochezia and epistaxis. She was recently hospitalized for an IBD flare at a local hospital with platelet decline from 150,000 to 44,000 during admission which improved on high-dose steroids. She was also noted to have Bacteroides fragilis bacteremia successfully treated with antibiotics.
On readmission, vitals were stable, and she appeared nontoxic. Labs showed Hgb 8.2 g/dL, platelets 2*10^3/µL, CRP 3.2, and albumin 2.8. CT revealed pancolitis. Sigmoidoscopy showed Mayo 3 disease and rectosigmoid narrowing (Figure 1). She was treated with high-dose steroids and IVIG for recurrent ITP. CMV viremia (PCR 20,611 IU/mL) with indeterminate colonic biopsy was noted. She responded to foscarnet and was discharged on valganciclovir, prolonged prednisone taper, and prophylactic trimethoprim-sulfamethoxazole.
Follow-up in the IBD clinic included infliximab (10 mg/kg) monotherapy induction with shared-decision making and a notable improvement in CRP, but she developed serum sickness-like reaction after two induction doses with undetectable antibodies and a week 2 level of 35 µg/mL. A DVT in her left lower extremity led to apixaban initiation. Limited steroid response led to upadacitinib initiation with clinical response and without ITP recurrence.
Discussion: ITP may develop from untreated or active UC via molecular mimicry but can also be triggered by infections. This case highlights ITP recurrence probably due to refractory UC and exacerbated by opportunistic CMV. A heightened index of suspicion is warranted to look for infections in the context of a flaring IBD patient with thrombocytopenia. Further research is needed to understand the interaction between UC and ITP to optimize management and understand infection interplay in these clinical scenarios.
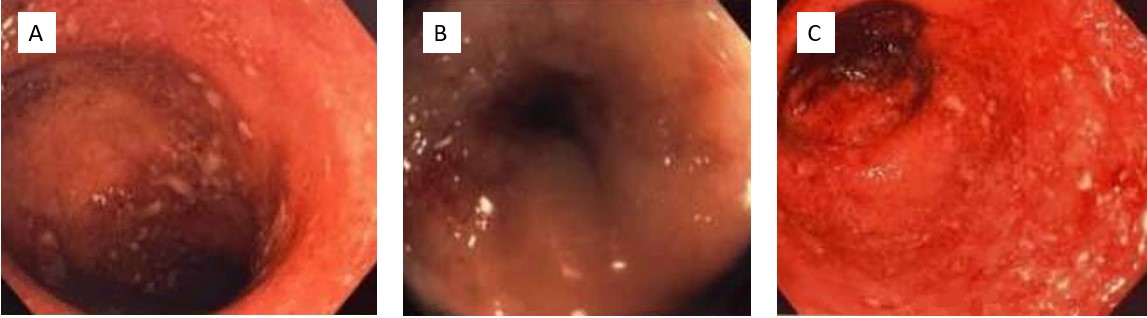
Figure: Figure 1. Sigmoidoscopy revealing Mayo 3 sigmoiditis (A), rectosigmoid narrowing (B), proctitis (C)
Disclosures:
Niraj Shah indicated no relevant financial relationships.
Sanket Patel: Abbvie – Speakers Bureau. BMS – Speakers Bureau. Lilly – Speakers Bureau. Pfizer – Speakers Bureau. Takeda – Speakers Bureau.
Niraj Shah, BS1, Sanket Patel, DO2. P2701 - A Rare Case of Immune Thrombocytopenic Purpura in the Setting of Ulcerative Colitis and Cytomegalovirus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
