Monday Poster Session
Category: IBD
P2705 - A Frequently Used Biologic Therapy With an Uncommon Ending
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- OR
Orlando Rodriguez-Amador, MD
VA Caribbean Healthcare System
San Juan, PR
Presenting Author(s)
Orlando Rodriguez-Amador, MD, Diego Roman-Colon, MD, Esteban Grovas-Cordovi, MD, Loscar Santiago-Rivera, MD
VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: Due to the accelerated pace in the advancement of the treatment of inflammatory bowel disease, it is important to understand their side effects and how to differentiate them from manifestation of the disease. They present with fever, pleuritic chest pain, and dyspnea. A commonly used therapy for IBD is Ustekinumab, an interleukin 12/23. Although described in literature, eosinophilic pneumonitis is a rare complication described in few cases. Here we present a case of a patient with Crohn’s disease who developed eosinophilic pneumonia after being treated with Ustekinumab.
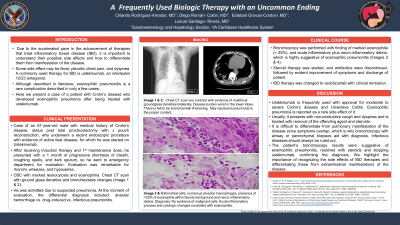
Case Description/Methods: An 81-year-old male with medical history of Crohn’s disease, s/p total proctocolectomy with J pouch reconstruction, who underwent a recent colonoscopy with evidence of active ileal disease, for which he was started on Ustekinumab. After receiving induction and 1st maintenance dose, he presented with a 1 month of progressive shortness of breath, coughing spells, and dark sputum, so he went to ED for evaluation. Evaluation was remarkable for rhonchi, wheezes, and hypoxemia. CBC with marked leukocytosis and eosinophilia. Chest CT with ground glass densities and bronchiectasis changes. He was admitted due to suspected pneumonia. At the moment of evaluation, differential included: alveolar hemorrhage vs. drug-induced vs. infectious pneumonitis. Bronchoscopy was performed with finding of marked eosinophilia ( > 25%), and acute inflammatory plus necro-inflammatory debris, highly suggestive of eosinophilic pneumonitis. Steroid therapy was started and antibiotics were discontinued, followed by improvement of symptoms and discharge of patient. IBD therapy was changed to vedolizumab with clinical remission.
Discussion: Ustekinumab is frequently used with approval for moderate to severe Crohn’s disease. Eosinophilic pneumonia is reported as a rare side effect of it. Usually it presents with non-productive cough and dyspnea and is treated with removal of the offending agent and steroids. It is difficult to differentiate from pulmonary manifestation of the disease since symptoms overlap, reason why bronchoscopy with airway or parenchymal biopsies aid with diagnosis. Infectious diseases should always be ruled out. The patient’s bronchoscopy results were suggestive of eosinophilic pneumonitis, resolved with steroids and stopping Ustekinumab, confirming the diagnosis. We highlight the importance of recognizing the side effects of IBD therapies and differentiating these from extraintestinal manifestations of the disease.
Disclosures:
Orlando Rodriguez-Amador, MD, Diego Roman-Colon, MD, Esteban Grovas-Cordovi, MD, Loscar Santiago-Rivera, MD. P2705 - A Frequently Used Biologic Therapy With an Uncommon Ending, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: Due to the accelerated pace in the advancement of the treatment of inflammatory bowel disease, it is important to understand their side effects and how to differentiate them from manifestation of the disease. They present with fever, pleuritic chest pain, and dyspnea. A commonly used therapy for IBD is Ustekinumab, an interleukin 12/23. Although described in literature, eosinophilic pneumonitis is a rare complication described in few cases. Here we present a case of a patient with Crohn’s disease who developed eosinophilic pneumonia after being treated with Ustekinumab.
Case Description/Methods: An 81-year-old male with medical history of Crohn’s disease, s/p total proctocolectomy with J pouch reconstruction, who underwent a recent colonoscopy with evidence of active ileal disease, for which he was started on Ustekinumab. After receiving induction and 1st maintenance dose, he presented with a 1 month of progressive shortness of breath, coughing spells, and dark sputum, so he went to ED for evaluation. Evaluation was remarkable for rhonchi, wheezes, and hypoxemia. CBC with marked leukocytosis and eosinophilia. Chest CT with ground glass densities and bronchiectasis changes. He was admitted due to suspected pneumonia. At the moment of evaluation, differential included: alveolar hemorrhage vs. drug-induced vs. infectious pneumonitis. Bronchoscopy was performed with finding of marked eosinophilia ( > 25%), and acute inflammatory plus necro-inflammatory debris, highly suggestive of eosinophilic pneumonitis. Steroid therapy was started and antibiotics were discontinued, followed by improvement of symptoms and discharge of patient. IBD therapy was changed to vedolizumab with clinical remission.
Discussion: Ustekinumab is frequently used with approval for moderate to severe Crohn’s disease. Eosinophilic pneumonia is reported as a rare side effect of it. Usually it presents with non-productive cough and dyspnea and is treated with removal of the offending agent and steroids. It is difficult to differentiate from pulmonary manifestation of the disease since symptoms overlap, reason why bronchoscopy with airway or parenchymal biopsies aid with diagnosis. Infectious diseases should always be ruled out. The patient’s bronchoscopy results were suggestive of eosinophilic pneumonitis, resolved with steroids and stopping Ustekinumab, confirming the diagnosis. We highlight the importance of recognizing the side effects of IBD therapies and differentiating these from extraintestinal manifestations of the disease.
Disclosures:
Orlando Rodriguez-Amador indicated no relevant financial relationships.
Diego Roman-Colon indicated no relevant financial relationships.
Esteban Grovas-Cordovi indicated no relevant financial relationships.
Loscar Santiago-Rivera indicated no relevant financial relationships.
Orlando Rodriguez-Amador, MD, Diego Roman-Colon, MD, Esteban Grovas-Cordovi, MD, Loscar Santiago-Rivera, MD. P2705 - A Frequently Used Biologic Therapy With an Uncommon Ending, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
