Monday Poster Session
Category: IBD
P2706 - HIV Screening Prior to Immune - Suppressive Therapy for Inflammatory Bowel Diseases: Essential or Optional?
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpeg.jpg)
Tarek Odah, MD
Mayo Clinic
Jacksonville, FL
Presenting Author(s)
Tarek Odah, MD, Maria Cristina Howard, MSN, Ewa M. Wysokinska, MD, Steven Attia, DO, Katherine J. Bodiford, MD, Julio C. Mendez, MD, Francis A. Farraye, MD, MSc, Jana G. Hashash, MD, MSc
Mayo Clinic, Jacksonville, FL
Introduction: Inflammatory bowel disease (IBD) management often includes immunosuppressive medications, raising the risk for opportunistic infections. We present a complex case of a patient with Crohn's disease (CD) who developed opportunistic infections, including recurrent candida esophagitis and Kaposi sarcoma, and HIV, after starting tumor necrosis factor (TNF) inhibitor and 6-mercaptopurine (6-MP) therapy.
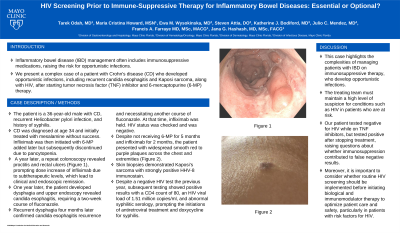
Case Description/Methods: The patient is a 36-year-old male with CD, recurrent Helicobacter pylori infection, and history of syphilis. CD was diagnosed at age 34 and initially treated with mesalamine without success. Infliximab was then initiated with 6-MP added later but subsequently discontinued due to pancytopenia. A year later, a repeat colonoscopy revealed proctitis and rectal ulcers, prompting dose increase of infliximab due to subtherapeutic levels, which lead to clinical and endoscopic remission. One year later, the patient developed dysphagia and upper endoscopy revealed candida esophagitis, requiring a two-week course of fluconazole. Recurrent dysphagia four months later confirmed candida esophagitis recurrence and necessitating another course of fluconazole. At that time, infliximab was held. HIV status was checked and was negative. Despite not receiving 6-MP for 5 months and infliximab for 2 months, the patient presented with widespread smooth red to purple plaques across the chest and extremities (Figure 1). Skin biopsies demonstrated Kaposi’s sarcoma with strongly positive HHV-8 immunostain. Despite a negative HIV test the previous year, subsequent testing showed positive results with a CD4 count of 80, an HIV viral load of 1.51 million copies/ml, and abnormal syphilitic serology, prompting the initiations of antiretroviral treatment and doxycycline for syphilis.
Discussion: This case highlights the complexities of managing patients with IBD on immunosuppressive therapy, who develop opportunistic infections. The treating team must maintain a high level of suspicion for conditions such as HIV in patients who are at risk. Our patient tested negative for HIV while on TNF inhibitors, but tested positive after stopping treatment, raising questions about whether immunosuppression contributed to false negative results. Moreover, it is important to consider whether routine HIV screening should be implemented before initiating biological and immunomodulator therapy to optimize patient care and safety, particularly in patients with risk factors for HIV.

Disclosures:
Tarek Odah, MD, Maria Cristina Howard, MSN, Ewa M. Wysokinska, MD, Steven Attia, DO, Katherine J. Bodiford, MD, Julio C. Mendez, MD, Francis A. Farraye, MD, MSc, Jana G. Hashash, MD, MSc. P2706 - HIV Screening Prior to Immune - Suppressive Therapy for Inflammatory Bowel Diseases: Essential or Optional?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Mayo Clinic, Jacksonville, FL
Introduction: Inflammatory bowel disease (IBD) management often includes immunosuppressive medications, raising the risk for opportunistic infections. We present a complex case of a patient with Crohn's disease (CD) who developed opportunistic infections, including recurrent candida esophagitis and Kaposi sarcoma, and HIV, after starting tumor necrosis factor (TNF) inhibitor and 6-mercaptopurine (6-MP) therapy.
Case Description/Methods: The patient is a 36-year-old male with CD, recurrent Helicobacter pylori infection, and history of syphilis. CD was diagnosed at age 34 and initially treated with mesalamine without success. Infliximab was then initiated with 6-MP added later but subsequently discontinued due to pancytopenia. A year later, a repeat colonoscopy revealed proctitis and rectal ulcers, prompting dose increase of infliximab due to subtherapeutic levels, which lead to clinical and endoscopic remission. One year later, the patient developed dysphagia and upper endoscopy revealed candida esophagitis, requiring a two-week course of fluconazole. Recurrent dysphagia four months later confirmed candida esophagitis recurrence and necessitating another course of fluconazole. At that time, infliximab was held. HIV status was checked and was negative. Despite not receiving 6-MP for 5 months and infliximab for 2 months, the patient presented with widespread smooth red to purple plaques across the chest and extremities (Figure 1). Skin biopsies demonstrated Kaposi’s sarcoma with strongly positive HHV-8 immunostain. Despite a negative HIV test the previous year, subsequent testing showed positive results with a CD4 count of 80, an HIV viral load of 1.51 million copies/ml, and abnormal syphilitic serology, prompting the initiations of antiretroviral treatment and doxycycline for syphilis.
Discussion: This case highlights the complexities of managing patients with IBD on immunosuppressive therapy, who develop opportunistic infections. The treating team must maintain a high level of suspicion for conditions such as HIV in patients who are at risk. Our patient tested negative for HIV while on TNF inhibitors, but tested positive after stopping treatment, raising questions about whether immunosuppression contributed to false negative results. Moreover, it is important to consider whether routine HIV screening should be implemented before initiating biological and immunomodulator therapy to optimize patient care and safety, particularly in patients with risk factors for HIV.

Figure: Figure 1: Kaposi's sarcoma
Disclosures:
Tarek Odah indicated no relevant financial relationships.
Maria Cristina Howard indicated no relevant financial relationships.
Ewa M. Wysokinska indicated no relevant financial relationships.
Steven Attia indicated no relevant financial relationships.
Katherine J. Bodiford indicated no relevant financial relationships.
Julio C. Mendez indicated no relevant financial relationships.
Francis Farraye: AbbVie – Consultant. Avalo Therapeutics – Consultant. Bausch – Advisor or Review Panel Member. BMS – Consultant. Braintree Labs – Consultant. DSMB for Lilly. – Sits on. Fresenius Kabi – Consultant. GI Reviewers and IBD Educational Group – independent contractor. GSK, Iterative Health, Janssen, Pfizer, Pharmacosmos, Sandoz Immunology, Sebela and Viatris – Consultant.
Jana Hashash: Bristol Myers Squibb – Consultant.
Tarek Odah, MD, Maria Cristina Howard, MSN, Ewa M. Wysokinska, MD, Steven Attia, DO, Katherine J. Bodiford, MD, Julio C. Mendez, MD, Francis A. Farraye, MD, MSc, Jana G. Hashash, MD, MSc. P2706 - HIV Screening Prior to Immune - Suppressive Therapy for Inflammatory Bowel Diseases: Essential or Optional?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
