Monday Poster Session
Category: IBD
P2708 - Active Ulcerative Colitis and Rectal Carcinoid Tumors: A Rare Occurrence
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Amla A. Patel, MBBS
Creighton University
Phoenix, AZ
Presenting Author(s)
Amla A. Patel, MBBS1, Ariana R. Tagliaferri, MD2, Andrew M. Weinberg, DO3
1Creighton University, Phoenix, AZ; 2Creighton University Medical Center, Phoenix, AZ; 3Creighton University School of Medicine, Scottsdale, AZ
Introduction: Rectal carcinoid tumors (RCTs) are rare lesions with an incidence of 0.17%. Chronic inflammation causes colonic epithelial dysplasia and leads to differentiation of pluripotent cells into neuroendocrine cells, and thus it can be questioned if the presence of IBD indirectly influences the pathogenesis of NETs. The presence of concomitant IBD and rectal carcinoid is very rare with only 11 cases currently described in literature; subsequently the treatment and prognosis of concomitant disease is poorly defined. We present a patient who underwent a colonoscopy for hematochezia and was found to have newly diagnosed ulcerative colitis and a RCT.
Case Description/Methods: A 50 YO F with tobacco use disorder underwent evaluation for subacute diffuse abdominal pain and bloody diarrhea. She was not anemic and denied constitutional symptoms. A CT A/P with IV contrast revealed rectal wall thickening with perirectal lymphadenopathy. A colonoscopy with adequate visualization revealed sigmoid diverticulosis with surrounding erythema, friable granular proctitis extending from the anus to 15 cm of scope insertion, and a 5 mm rectal polyp removed via hot snare polypectomy. Sigmoid and rectal biopsies revealed inflamed mucosa with active cryptitis and mild architectural distortion with crypt branching, diagnostic of ulcerative proctocolitis. The rectal polyp was pathologically a Grade I, well-differentiated carcinoid tumor with moderate active colitis and architectural distortion. She was prescribed oral mesalamine 2.4 g for one month, but given ongoing symptoms she was treated with a 6-week prednisone taper and mesalamine 4 g rectal enemas. After 6 months of refractory symptoms, she was started on induction-dosing of vedolizumab 300 mg (0,2,6 week intervals) and then every 8 weeks for maintenance. She will undergo a colonoscopy 1 year from diagnosis for IBD surveillance.
Discussion: The treatment of RCTs are based on the size (>1 cm) and degree of mitotic activity (Ki67 >3%) which confer a higher rate of malignant transformation. Endoscopic versus surgical resection is debated. Low-grade lesions do not require post-resection surveillance, as in our patient. With the histological remission of IBD, NETs may spontaneously regress, again suggesting that IBD plays a role in the pathogenesis. While the management of RCTs alone is well-defined in current literature, the treatment and surveillance of concomitant disease is poorly understood.

Disclosures:
Amla A. Patel, MBBS1, Ariana R. Tagliaferri, MD2, Andrew M. Weinberg, DO3. P2708 - Active Ulcerative Colitis and Rectal Carcinoid Tumors: A Rare Occurrence, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Creighton University, Phoenix, AZ; 2Creighton University Medical Center, Phoenix, AZ; 3Creighton University School of Medicine, Scottsdale, AZ
Introduction: Rectal carcinoid tumors (RCTs) are rare lesions with an incidence of 0.17%. Chronic inflammation causes colonic epithelial dysplasia and leads to differentiation of pluripotent cells into neuroendocrine cells, and thus it can be questioned if the presence of IBD indirectly influences the pathogenesis of NETs. The presence of concomitant IBD and rectal carcinoid is very rare with only 11 cases currently described in literature; subsequently the treatment and prognosis of concomitant disease is poorly defined. We present a patient who underwent a colonoscopy for hematochezia and was found to have newly diagnosed ulcerative colitis and a RCT.
Case Description/Methods: A 50 YO F with tobacco use disorder underwent evaluation for subacute diffuse abdominal pain and bloody diarrhea. She was not anemic and denied constitutional symptoms. A CT A/P with IV contrast revealed rectal wall thickening with perirectal lymphadenopathy. A colonoscopy with adequate visualization revealed sigmoid diverticulosis with surrounding erythema, friable granular proctitis extending from the anus to 15 cm of scope insertion, and a 5 mm rectal polyp removed via hot snare polypectomy. Sigmoid and rectal biopsies revealed inflamed mucosa with active cryptitis and mild architectural distortion with crypt branching, diagnostic of ulcerative proctocolitis. The rectal polyp was pathologically a Grade I, well-differentiated carcinoid tumor with moderate active colitis and architectural distortion. She was prescribed oral mesalamine 2.4 g for one month, but given ongoing symptoms she was treated with a 6-week prednisone taper and mesalamine 4 g rectal enemas. After 6 months of refractory symptoms, she was started on induction-dosing of vedolizumab 300 mg (0,2,6 week intervals) and then every 8 weeks for maintenance. She will undergo a colonoscopy 1 year from diagnosis for IBD surveillance.
Discussion: The treatment of RCTs are based on the size (>1 cm) and degree of mitotic activity (Ki67 >3%) which confer a higher rate of malignant transformation. Endoscopic versus surgical resection is debated. Low-grade lesions do not require post-resection surveillance, as in our patient. With the histological remission of IBD, NETs may spontaneously regress, again suggesting that IBD plays a role in the pathogenesis. While the management of RCTs alone is well-defined in current literature, the treatment and surveillance of concomitant disease is poorly understood.

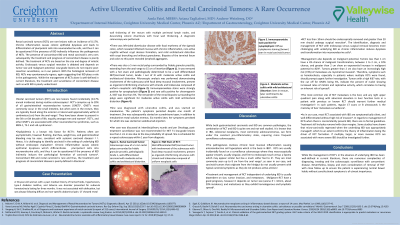
Figure: Figure 1. Rectal Carcinoid Tumor: Colonoscopic view of a 5 mm rectal polyp surrounded by friable granular proctitis, pathologically Grade 1, well-differentiated carcinoid with moderate active colitis and architectural distortion.
Disclosures:
Amla Patel indicated no relevant financial relationships.
Ariana Tagliaferri indicated no relevant financial relationships.
Andrew Weinberg indicated no relevant financial relationships.
Amla A. Patel, MBBS1, Ariana R. Tagliaferri, MD2, Andrew M. Weinberg, DO3. P2708 - Active Ulcerative Colitis and Rectal Carcinoid Tumors: A Rare Occurrence, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
