Monday Poster Session
Category: IBD
P2618 - Polypharmacy in Inflammatory Bowel Disease: Systematic Review and Meta-analysis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Mouhand F.H Mohamed, MD, MSc
Mayo Clinic
Rochester, MN
Presenting Author(s)
Mouhand F.H. Mohamed, MD, MSc1, Michelle Kwon, MD2, Azizullah Beran, MD3, Khaled Elfert, MD4, Samir A. Shah, MD5
1Mayo Clinic, Rochester, MN; 2Brown University / Warren Alpert Medical School, Providence, RI; 3Indiana University School of Medicine, Indianapolis, IN; 4West Virginia University, Morgantown, WV; 5Gastroenterology Associates, Inc., powered by GI Alliance, Providence, RI
Introduction: Polypharmacy (PP), or the concurrent use of multiple medications, is increasingly prevalent. PP raises significant concerns, including drug-drug interactions, adverse drug reactions, potentially lower medication adherence, and increased healthcare costs. This meta-analysis evaluates the PP burden in Inflammatory Bowel Disease (IBD).
Methods: We comprehensively searched PubMed and EMBASE until November 2023 to identify studies reporting PP prevalence in adult (> 18 Y) patients with IBD. Based on a scoping review of the literature, we defined PP in three levels: any PP (concurrent use of > 2 drugs), moderate PP (concurrent use of > 5 drugs), and severe PP (concurrent use of > 10 drugs). The primary outcome of our study was the prevalence of moderate PP. The random effects model was used to pool PP prevalence with its 95% Confidence Interval (CI). I2 was used to adjudicate heterogeneity.
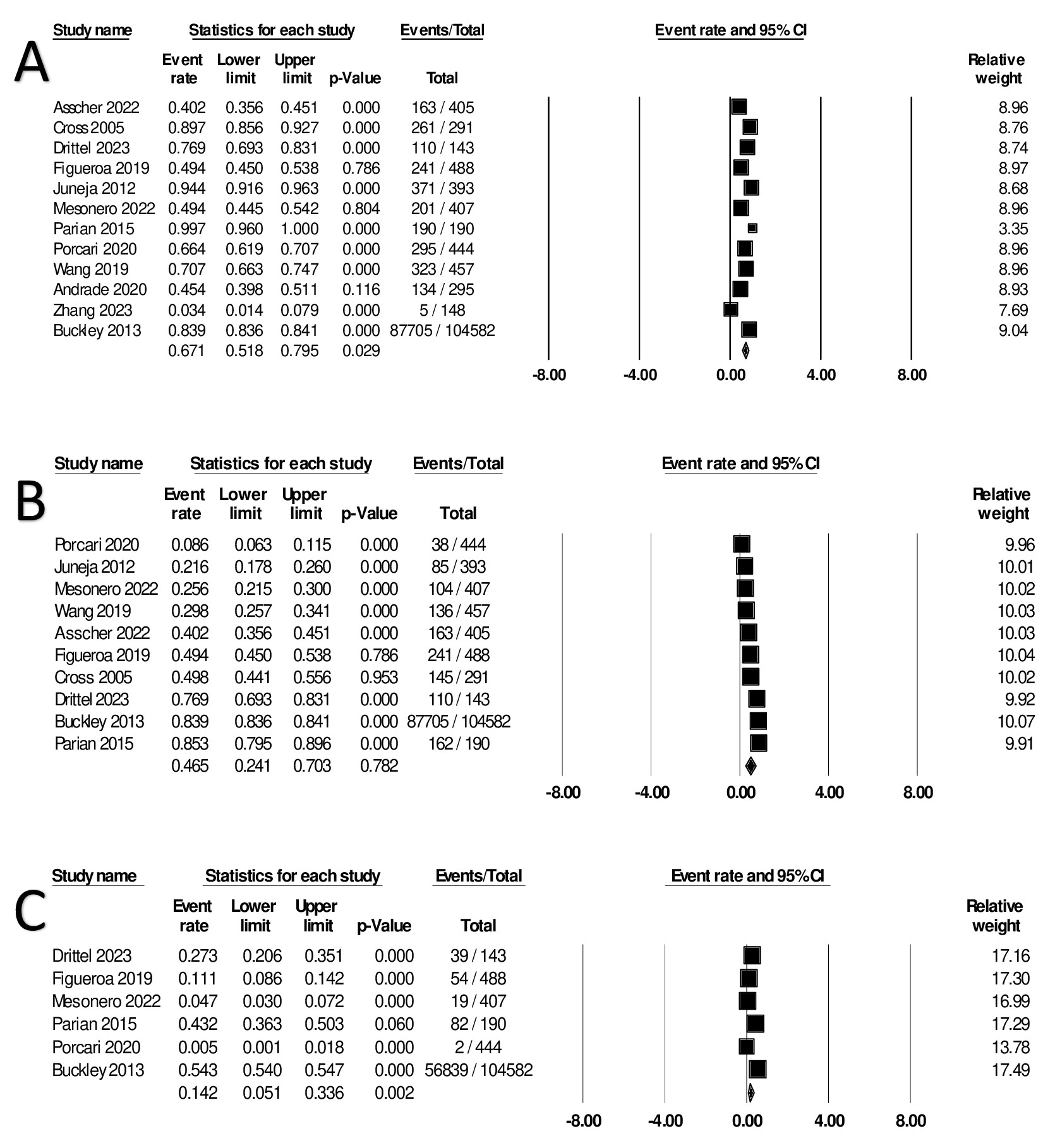
Results: Twelve studies (108,243 patients) were included in our final analysis. Buckley et al. study contributed the majority of patients (104,582). The PP prevalence varied according to the criteria of included studies, which differed in aspects like the definition of PP, consideration of over-the-counter drugs, and specific IBD medications. The global prevalence of any PP was 67.13% (95% CI: 51.84% - 79.49%, I2 98%). The prevalence was higher in the United States (US), 83.75% (95% CI: 72.03% - 91.16%, I2 98%). The global rate for moderate PP was 46.47% (95% CI: 24.13% - 70.32%, I2 99%) and was higher in the US, 58.51% (95% CI: 32.4-80.55%, I2 99%). Severe PP prevalence globally was 14.16% (95% CI: 5.11% - 33.56%, I2 99%), compared to 31.29% in the US (95% CI: 13.50% - 57.06%, I2 98%). A sensitivity analysis excluding Buckley et al.'s study revealed similar results.
Discussion: This study revealed a substantial burden of polypharmacy in patients with IBD. The PP varied between studies, likely due to differences in the PP definition and population studied. This variability highlights the complexity of medication management in IBD. Further studies are needed to understand and address the challenges posed by polypharmacy.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mouhand F.H. Mohamed, MD, MSc1, Michelle Kwon, MD2, Azizullah Beran, MD3, Khaled Elfert, MD4, Samir A. Shah, MD5. P2618 - Polypharmacy in Inflammatory Bowel Disease: Systematic Review and Meta-analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mayo Clinic, Rochester, MN; 2Brown University / Warren Alpert Medical School, Providence, RI; 3Indiana University School of Medicine, Indianapolis, IN; 4West Virginia University, Morgantown, WV; 5Gastroenterology Associates, Inc., powered by GI Alliance, Providence, RI
Introduction: Polypharmacy (PP), or the concurrent use of multiple medications, is increasingly prevalent. PP raises significant concerns, including drug-drug interactions, adverse drug reactions, potentially lower medication adherence, and increased healthcare costs. This meta-analysis evaluates the PP burden in Inflammatory Bowel Disease (IBD).
Methods: We comprehensively searched PubMed and EMBASE until November 2023 to identify studies reporting PP prevalence in adult (> 18 Y) patients with IBD. Based on a scoping review of the literature, we defined PP in three levels: any PP (concurrent use of > 2 drugs), moderate PP (concurrent use of > 5 drugs), and severe PP (concurrent use of > 10 drugs). The primary outcome of our study was the prevalence of moderate PP. The random effects model was used to pool PP prevalence with its 95% Confidence Interval (CI). I2 was used to adjudicate heterogeneity.
Results: Twelve studies (108,243 patients) were included in our final analysis. Buckley et al. study contributed the majority of patients (104,582). The PP prevalence varied according to the criteria of included studies, which differed in aspects like the definition of PP, consideration of over-the-counter drugs, and specific IBD medications. The global prevalence of any PP was 67.13% (95% CI: 51.84% - 79.49%, I2 98%). The prevalence was higher in the United States (US), 83.75% (95% CI: 72.03% - 91.16%, I2 98%). The global rate for moderate PP was 46.47% (95% CI: 24.13% - 70.32%, I2 99%) and was higher in the US, 58.51% (95% CI: 32.4-80.55%, I2 99%). Severe PP prevalence globally was 14.16% (95% CI: 5.11% - 33.56%, I2 99%), compared to 31.29% in the US (95% CI: 13.50% - 57.06%, I2 98%). A sensitivity analysis excluding Buckley et al.'s study revealed similar results.
Discussion: This study revealed a substantial burden of polypharmacy in patients with IBD. The PP varied between studies, likely due to differences in the PP definition and population studied. This variability highlights the complexity of medication management in IBD. Further studies are needed to understand and address the challenges posed by polypharmacy.
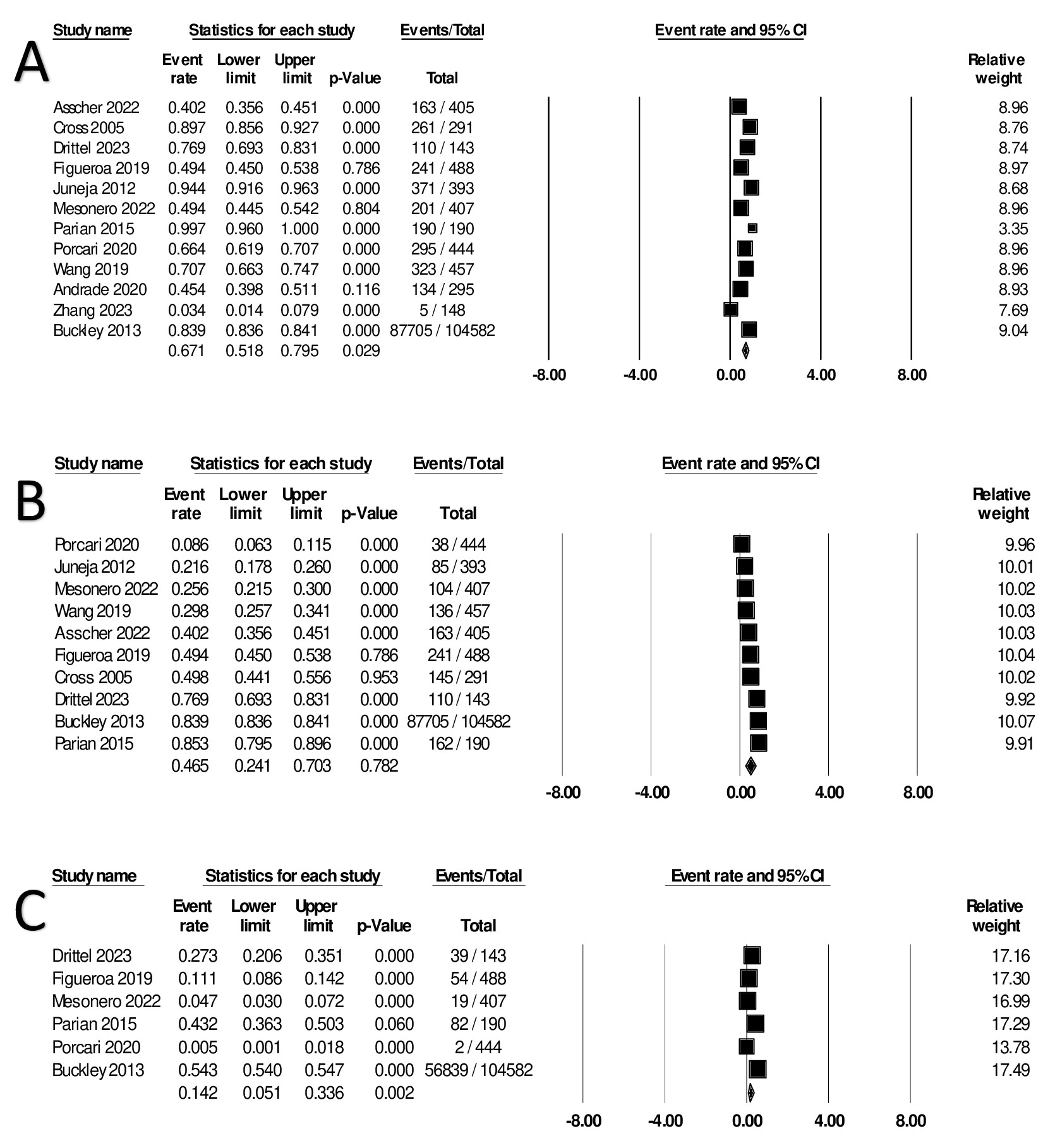
Figure: Figure 1: Forrest plot summarizing the prevalence of A) any polypharmacy (use of > 2 drugs), B) moderate PP (use of > 5 drugs), and C) severe PP (use of > 10 drugs)
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mouhand Mohamed indicated no relevant financial relationships.
Michelle Kwon indicated no relevant financial relationships.
Azizullah Beran indicated no relevant financial relationships.
Khaled Elfert indicated no relevant financial relationships.
Samir Shah: Roche Information Systems – Consultant.
Mouhand F.H. Mohamed, MD, MSc1, Michelle Kwon, MD2, Azizullah Beran, MD3, Khaled Elfert, MD4, Samir A. Shah, MD5. P2618 - Polypharmacy in Inflammatory Bowel Disease: Systematic Review and Meta-analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
