Monday Poster Session
Category: IBD
P2549 - The Effects of Social Determinants of Health on Medication Utilization in Patients With Inflammatory Bowel Disease
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Maryana Stryelkina, DO
Baylor Scott & White Medical Center
Temple, TX
Presenting Author(s)
Maryana Stryelkina, DO1, Megan Lewis, MD1, Eric Smith, MD2, Rajesh Shah, MD, MS3
1Baylor Scott & White Medical Center, Temple, TX; 2Baylor Scott & White Medical Center, Round Rock, TX; 3Baylor Scott & White Medical Center, Buda, TX
Introduction: Inflammatory bowel diseases (IBD), including ulcerative colitis (UC) and Crohn's disease (CD), are chronic inflammatory disorders requiring significant healthcare utilization. Studies have suggested variations in healthcare utilization across racial and ethnic groups, with minorities experiencing higher rates of complications, hospitalizations, and surgeries. However, there are limited studies into the influence of social determinants of health (SDOH), such as financial security, transportation and food security, on medication utilization. This study aimed to examine the effects of SDOH factors on medication utilization in adult patients with IBD.
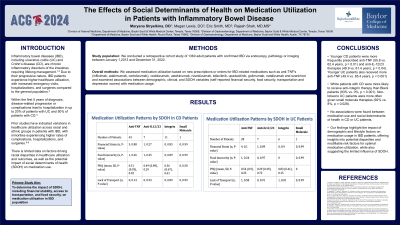
Methods: We conducted a retrospective cohort study of 1,360 adult IBD patients (UC and CD) who received care within the Baylor Scott and White Healthcare system. We assessed medication utilization based on new prescriptions or orders for IBD-related medications (anti-TNFs, anti-integrins, anti-IL-12/23 and small molecules) and examined associations between demographic, clinical, and SDOH variables (self-reported financial security, food security, transportation and depression scores) with medication usage.
Results: Younger patients with CD were more likely to be prescribed anti-TNF (55.8 vs 62.4 years, P=0.01) and anti-IL-12/23 medications (49.9 vs 61.4 years, p=0.04). Similarly, younger patients with UC were more likely to receive anti-TNF therapy (49.4 vs 65.4 years, p < 0.001). In terms of race, White patients were more likely to receive anti-integrin therapies compared to Black patients with CD (83% vs 0%, p < 0.001). In patients with UC, non-tobacco users received small molecule therapy more often than tobacco users (92% vs 8%, p= 0.028). Medication utilization was not significantly associated with SDOH factors including financial strain, food insecurity, transportation, or depression severity in either UC or CD patients.
Discussion: These findings highlight the impact of demographic and lifestyle factors on medication usage in IBD patients, offering insights into potential disparities and modifiable risk factors for optimal medication utilization, while also suggesting the limited influence of SDOH on medication utilization.
Disclosures:
Maryana Stryelkina, DO1, Megan Lewis, MD1, Eric Smith, MD2, Rajesh Shah, MD, MS3. P2549 - The Effects of Social Determinants of Health on Medication Utilization in Patients With Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Baylor Scott & White Medical Center, Temple, TX; 2Baylor Scott & White Medical Center, Round Rock, TX; 3Baylor Scott & White Medical Center, Buda, TX
Introduction: Inflammatory bowel diseases (IBD), including ulcerative colitis (UC) and Crohn's disease (CD), are chronic inflammatory disorders requiring significant healthcare utilization. Studies have suggested variations in healthcare utilization across racial and ethnic groups, with minorities experiencing higher rates of complications, hospitalizations, and surgeries. However, there are limited studies into the influence of social determinants of health (SDOH), such as financial security, transportation and food security, on medication utilization. This study aimed to examine the effects of SDOH factors on medication utilization in adult patients with IBD.
Methods: We conducted a retrospective cohort study of 1,360 adult IBD patients (UC and CD) who received care within the Baylor Scott and White Healthcare system. We assessed medication utilization based on new prescriptions or orders for IBD-related medications (anti-TNFs, anti-integrins, anti-IL-12/23 and small molecules) and examined associations between demographic, clinical, and SDOH variables (self-reported financial security, food security, transportation and depression scores) with medication usage.
Results: Younger patients with CD were more likely to be prescribed anti-TNF (55.8 vs 62.4 years, P=0.01) and anti-IL-12/23 medications (49.9 vs 61.4 years, p=0.04). Similarly, younger patients with UC were more likely to receive anti-TNF therapy (49.4 vs 65.4 years, p < 0.001). In terms of race, White patients were more likely to receive anti-integrin therapies compared to Black patients with CD (83% vs 0%, p < 0.001). In patients with UC, non-tobacco users received small molecule therapy more often than tobacco users (92% vs 8%, p= 0.028). Medication utilization was not significantly associated with SDOH factors including financial strain, food insecurity, transportation, or depression severity in either UC or CD patients.
Discussion: These findings highlight the impact of demographic and lifestyle factors on medication usage in IBD patients, offering insights into potential disparities and modifiable risk factors for optimal medication utilization, while also suggesting the limited influence of SDOH on medication utilization.
Disclosures:
Maryana Stryelkina indicated no relevant financial relationships.
Megan Lewis indicated no relevant financial relationships.
Eric Smith indicated no relevant financial relationships.
Rajesh Shah indicated no relevant financial relationships.
Maryana Stryelkina, DO1, Megan Lewis, MD1, Eric Smith, MD2, Rajesh Shah, MD, MS3. P2549 - The Effects of Social Determinants of Health on Medication Utilization in Patients With Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
