Monday Poster Session
Category: GI Bleeding
P2469 - Outdated Preventive Measures for Aspirin Leading to Gastrointestinal Complications: A Propensity-Matched Cohort Study
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Taimur S. Muzammil, MD
Allegheny General Hospital
Pittsburgh, PA
Presenting Author(s)
Taimur S. Muzammil, MD, Himsikhar Khataniar, MD, Muhammad Ali Butt, MD, Balaji Jagdish, DO, Omar Al'Taani, MD
Allegheny General Hospital, Pittsburgh, PA
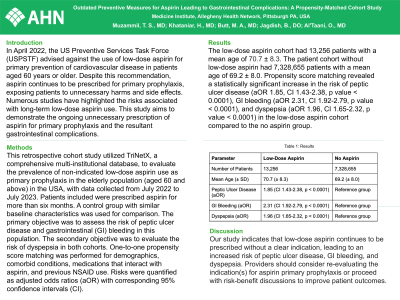
Introduction: In April 2022, the US Preventive Services Task Force (USPSTF) advised against the use of low-dose aspirin for primary prevention of cardiovascular disease in patients aged 60 years or older. Despite this recommendation, aspirin continues to be prescribed for primary prophylaxis, exposing patients to unnecessary harms and side effects. Numerous studies have highlighted the risks associated with long-term low-dose aspirin use. This study aims to demonstrate the ongoing unnecessary prescription of aspirin for primary prophylaxis and the resultant gastrointestinal complications.
Methods: This retrospective cohort study utilized TriNetX, a comprehensive multi-institutional database, to evaluate the prevalence of non-indicated low-dose aspirin use as primary prophylaxis in the elderly population (aged 60 and above) in the USA, with data collected from July 2022 to July 2023. Patients included were prescribed aspirin for more than six months. A control group with similar baseline characteristics was used for comparison. The primary objective was to assess the risk of peptic ulcer disease and gastrointestinal (GI) bleeding in this population. The secondary objective was to evaluate the risk of dyspepsia in both cohorts. One-to-one propensity score matching was performed for demographics, comorbid conditions, medications that interact with aspirin, and previous NSAID use. Risks were quantified as adjusted odds ratios (aOR) with corresponding 95% confidence intervals (CI).
Results: The low-dose aspirin cohort had 13,256 patients with a mean age of 70.7 ± 8.3. The patient cohort without low-dose aspirin had 7,328,655 patients with a mean age of 69.2 ± 8.0. Propensity score matching revealed a statistically significant increase in the risk of peptic ulcer disease (aOR 1.85, CI 1.43-2.38, p value < 0.0001), GI bleeding (aOR 2.31, CI 1.92-2.79, p value < 0.0001), and dyspepsia (aOR 1.96, CI 1.65-2.32, p value < 0.0001) in the low-dose aspirin cohort compared to the no aspirin group.
Discussion: Our study indicates that low-dose aspirin continues to be prescribed without a clear indication, leading to an increased risk of peptic ulcer disease, GI bleeding, and dyspepsia. Providers should consider re-evaluating the indication(s) for aspirin primary prophylaxis or proceed with risk-benefit discussions to improve patient outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Taimur S. Muzammil, MD, Himsikhar Khataniar, MD, Muhammad Ali Butt, MD, Balaji Jagdish, DO, Omar Al'Taani, MD. P2469 - Outdated Preventive Measures for Aspirin Leading to Gastrointestinal Complications: A Propensity-Matched Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Allegheny General Hospital, Pittsburgh, PA
Introduction: In April 2022, the US Preventive Services Task Force (USPSTF) advised against the use of low-dose aspirin for primary prevention of cardiovascular disease in patients aged 60 years or older. Despite this recommendation, aspirin continues to be prescribed for primary prophylaxis, exposing patients to unnecessary harms and side effects. Numerous studies have highlighted the risks associated with long-term low-dose aspirin use. This study aims to demonstrate the ongoing unnecessary prescription of aspirin for primary prophylaxis and the resultant gastrointestinal complications.
Methods: This retrospective cohort study utilized TriNetX, a comprehensive multi-institutional database, to evaluate the prevalence of non-indicated low-dose aspirin use as primary prophylaxis in the elderly population (aged 60 and above) in the USA, with data collected from July 2022 to July 2023. Patients included were prescribed aspirin for more than six months. A control group with similar baseline characteristics was used for comparison. The primary objective was to assess the risk of peptic ulcer disease and gastrointestinal (GI) bleeding in this population. The secondary objective was to evaluate the risk of dyspepsia in both cohorts. One-to-one propensity score matching was performed for demographics, comorbid conditions, medications that interact with aspirin, and previous NSAID use. Risks were quantified as adjusted odds ratios (aOR) with corresponding 95% confidence intervals (CI).
Results: The low-dose aspirin cohort had 13,256 patients with a mean age of 70.7 ± 8.3. The patient cohort without low-dose aspirin had 7,328,655 patients with a mean age of 69.2 ± 8.0. Propensity score matching revealed a statistically significant increase in the risk of peptic ulcer disease (aOR 1.85, CI 1.43-2.38, p value < 0.0001), GI bleeding (aOR 2.31, CI 1.92-2.79, p value < 0.0001), and dyspepsia (aOR 1.96, CI 1.65-2.32, p value < 0.0001) in the low-dose aspirin cohort compared to the no aspirin group.
Discussion: Our study indicates that low-dose aspirin continues to be prescribed without a clear indication, leading to an increased risk of peptic ulcer disease, GI bleeding, and dyspepsia. Providers should consider re-evaluating the indication(s) for aspirin primary prophylaxis or proceed with risk-benefit discussions to improve patient outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Taimur Muzammil indicated no relevant financial relationships.
Himsikhar Khataniar indicated no relevant financial relationships.
Muhammad Ali Butt indicated no relevant financial relationships.
Balaji Jagdish indicated no relevant financial relationships.
Omar Al'Taani indicated no relevant financial relationships.
Taimur S. Muzammil, MD, Himsikhar Khataniar, MD, Muhammad Ali Butt, MD, Balaji Jagdish, DO, Omar Al'Taani, MD. P2469 - Outdated Preventive Measures for Aspirin Leading to Gastrointestinal Complications: A Propensity-Matched Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
