Monday Poster Session
Category: GI Bleeding
P2470 - When It Bleeds, It Pours: Esophageal Dieulafoy’s Lesion - First Systematic Review Evaluating Diagnostic and Therapeutic Conundrums
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MA
Muhammad Sajeel Anwar, MD
UHS Wilson Medical Center
Johnson City, NY
Presenting Author(s)
Faisal Inayat, MBBS1, Muhammad Sajeel Anwar, MD2, Ahtshamullah Chaudhry, MD3, Faisal Ibrahim, MBBS4, Gul Nawaz, MD5
1Allama Iqbal Medical College, Lahore, Punjab, Pakistan; 2UHS Wilson Medical Center, Johnson City, NY; 3St. Dominic's Hospital, Jackson, MS; 4Wexham Park Hospital, Slough, England, United Kingdom; 5Marshfield Medical Center, Marshfield, WI
Introduction: Esophageal Dieulafoy's lesion consists of an abnormally large, tortuous, submucosal arterial vessel, which protrudes into the mucosa through minimal weaknesses in continuity. This elusive clinicopathologic entity may cause massive upper gastrointestinal bleeding, leading to hemodynamic compromise. Published literature remains limited, mainly consisting of case reports or small case series.
Methods: We conducted a systematic literature search of MEDLINE (PubMed and Ovid), Cochrane, Scopus, and Google Scholar databases following PRISMA guidelines. Adult ( >18 years old) human case reports of esophageal Dieulafoy’s lesion were searched. No time restrictions were applied. The latest search date was June 05, 2024. Specific search terminologies, such as ''Dieulafoy’s lesion,'' ''Dieulafoy,'' and ''Exulceratio Simplex'' were combined using the Boolean operators ''AND'' and ''OR'' with ''esophagus'' and ''esophageal,'' with all relevant permutations.
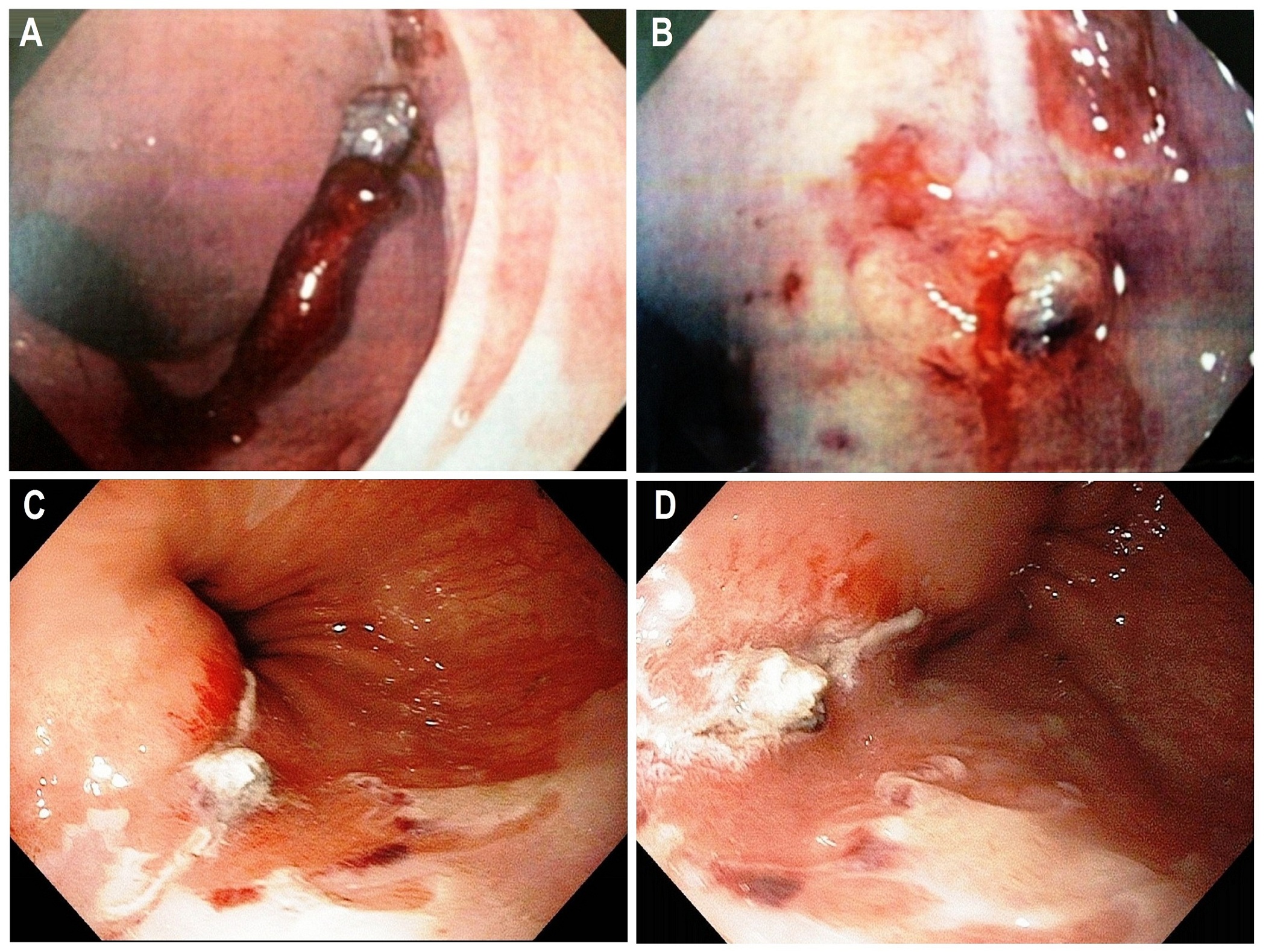
Results: A total of 28 case reports (level of clinical evidence: IV) dating from 1994 to 2023 were identified. The mean age of presentation was 58.8 ± 17.1 years (range, 24-92 years), with 78.5% of cases reported in males. Clinical presentations included hematemesis in 53.6%, combined hematemesis and melena in 25%, melena in 14.3%, and hemodynamic compromise in 10.7% of patients. Major underlying disorders were diabetes mellitus 39.2%, hypertension 28.6%, chronic kidney disease 17.8%, and coronary artery disease 14.3%. Mean admission hemoglobin level was 7.2 ± 2.6 mg/dL. Esophagogastroduodenoscopy (96.4%) was the mainstay of diagnosis. The lesion most commonly affected the distal esophagus (57.1%), followed by the mid (35.7%) and upper (7.1%) parts (Figure 1). Treatment included combination endoscopic therapy with epinephrine injection plus hemoclip placement (46.4%), hemoclipping alone (25%), band ligation (10.7%), and electrocoagulation (14.3%). The endoscopic therapeutic approach was a feasible choice for esophageal disease, with a primary hemostasis rate of 97%. The overall mortality rate was 3.6%.
Discussion: This systematic review illustrates that esophageal Dieulafoy’s lesion remains a rare diagnosis. Prompt detection and appropriate management are of paramount importance to prevent serious hemodynamic complications. The best treatment modality remains to be determined, but the data presented here support the use of an endoscopic combination therapy using epinephrine injection followed by hemoclipping as safe and effective.
Disclosures:
Faisal Inayat, MBBS1, Muhammad Sajeel Anwar, MD2, Ahtshamullah Chaudhry, MD3, Faisal Ibrahim, MBBS4, Gul Nawaz, MD5. P2470 - When It Bleeds, It Pours: Esophageal Dieulafoy’s Lesion - First Systematic Review Evaluating Diagnostic and Therapeutic Conundrums, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Allama Iqbal Medical College, Lahore, Punjab, Pakistan; 2UHS Wilson Medical Center, Johnson City, NY; 3St. Dominic's Hospital, Jackson, MS; 4Wexham Park Hospital, Slough, England, United Kingdom; 5Marshfield Medical Center, Marshfield, WI
Introduction: Esophageal Dieulafoy's lesion consists of an abnormally large, tortuous, submucosal arterial vessel, which protrudes into the mucosa through minimal weaknesses in continuity. This elusive clinicopathologic entity may cause massive upper gastrointestinal bleeding, leading to hemodynamic compromise. Published literature remains limited, mainly consisting of case reports or small case series.
Methods: We conducted a systematic literature search of MEDLINE (PubMed and Ovid), Cochrane, Scopus, and Google Scholar databases following PRISMA guidelines. Adult ( >18 years old) human case reports of esophageal Dieulafoy’s lesion were searched. No time restrictions were applied. The latest search date was June 05, 2024. Specific search terminologies, such as ''Dieulafoy’s lesion,'' ''Dieulafoy,'' and ''Exulceratio Simplex'' were combined using the Boolean operators ''AND'' and ''OR'' with ''esophagus'' and ''esophageal,'' with all relevant permutations.
Results: A total of 28 case reports (level of clinical evidence: IV) dating from 1994 to 2023 were identified. The mean age of presentation was 58.8 ± 17.1 years (range, 24-92 years), with 78.5% of cases reported in males. Clinical presentations included hematemesis in 53.6%, combined hematemesis and melena in 25%, melena in 14.3%, and hemodynamic compromise in 10.7% of patients. Major underlying disorders were diabetes mellitus 39.2%, hypertension 28.6%, chronic kidney disease 17.8%, and coronary artery disease 14.3%. Mean admission hemoglobin level was 7.2 ± 2.6 mg/dL. Esophagogastroduodenoscopy (96.4%) was the mainstay of diagnosis. The lesion most commonly affected the distal esophagus (57.1%), followed by the mid (35.7%) and upper (7.1%) parts (Figure 1). Treatment included combination endoscopic therapy with epinephrine injection plus hemoclip placement (46.4%), hemoclipping alone (25%), band ligation (10.7%), and electrocoagulation (14.3%). The endoscopic therapeutic approach was a feasible choice for esophageal disease, with a primary hemostasis rate of 97%. The overall mortality rate was 3.6%.
Discussion: This systematic review illustrates that esophageal Dieulafoy’s lesion remains a rare diagnosis. Prompt detection and appropriate management are of paramount importance to prevent serious hemodynamic complications. The best treatment modality remains to be determined, but the data presented here support the use of an endoscopic combination therapy using epinephrine injection followed by hemoclipping as safe and effective.
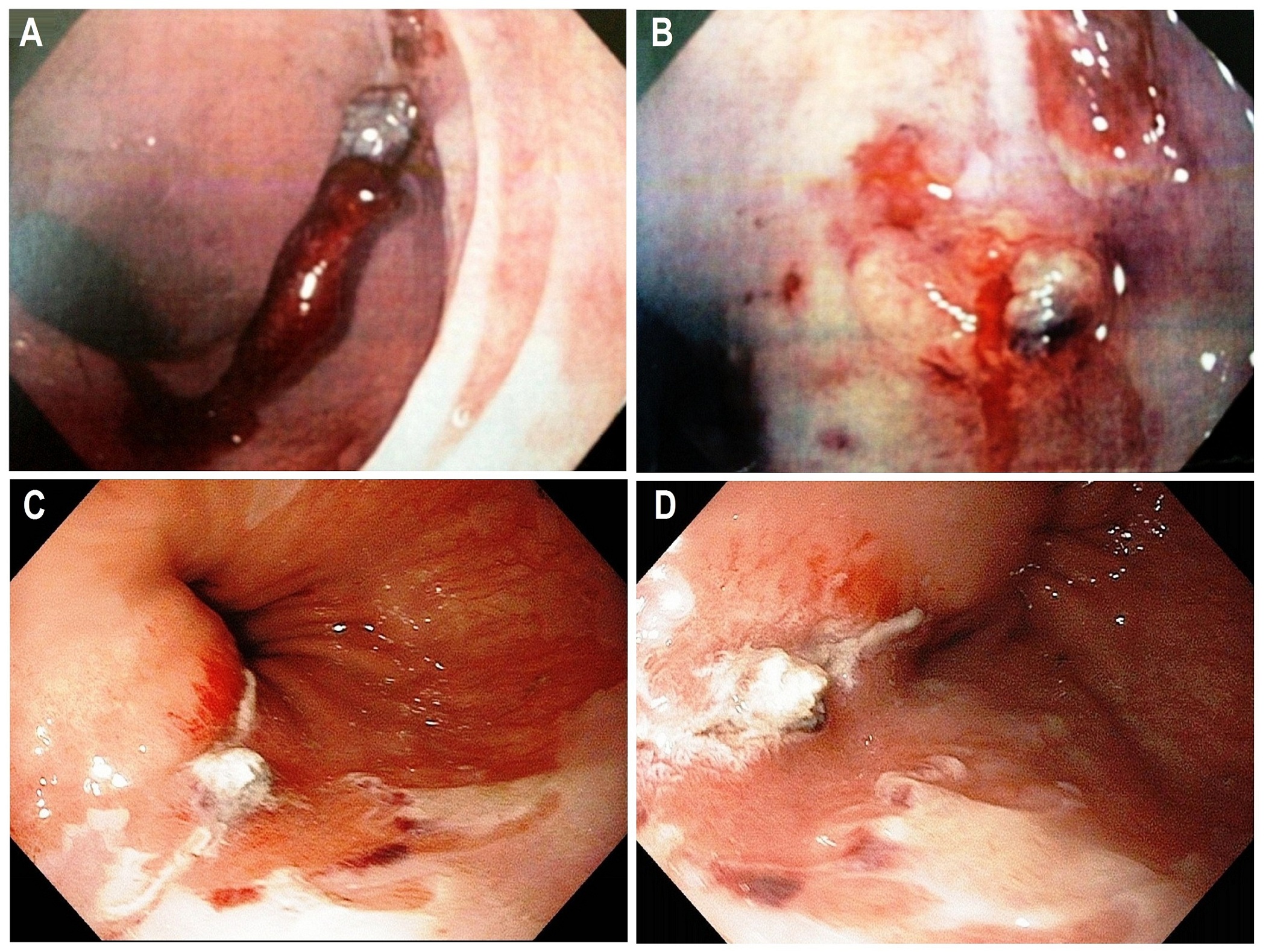
Figure: Figure 1. Esophagogastroduodenoscopy findings in esophageal Dieulafoy’s lesion. Panel A: An adherent clot in distal esophagus. Panel B: A vessel was seen protruding into the esophageal lumen without surrounding ulceration. Panels C and D: A vessel protruding into the lumen of the distal esophagus.
Disclosures:
Faisal Inayat indicated no relevant financial relationships.
Muhammad Sajeel Anwar indicated no relevant financial relationships.
Ahtshamullah Chaudhry indicated no relevant financial relationships.
Faisal Ibrahim indicated no relevant financial relationships.
Gul Nawaz indicated no relevant financial relationships.
Faisal Inayat, MBBS1, Muhammad Sajeel Anwar, MD2, Ahtshamullah Chaudhry, MD3, Faisal Ibrahim, MBBS4, Gul Nawaz, MD5. P2470 - When It Bleeds, It Pours: Esophageal Dieulafoy’s Lesion - First Systematic Review Evaluating Diagnostic and Therapeutic Conundrums, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
