Monday Poster Session
Category: GI Bleeding
P2476 - Skin Cancer Where the Sun Doesn’t Shine: A Rare Case of Anorectal Melanoma
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- JG
Julia E. Gallagher, BA
University of South Florida
Tampa, FL
Presenting Author(s)
Julia E. Gallagher, BA1, Heather Gosnell, DO2, Bharat Ponnaganti, MD1, Matthew Heckroth, MD1, Aditi Saha, MBBS1, Vita Saranga-Perry, MD3, Jeffrey A. Kooper, MD4, William Bulkeley, MD5, Jonathan Keshishian, MD5
1University of South Florida, Tampa, FL; 2University of South Florida Morsani College of Medicine, Tampa, FL; 3Tampa General Hospital / University of South Florida, Tampa, FL; 4University of South Florida, James A. Haley VA Hospital, Tampa, FL; 5James A. Haley Veterans' Hospital, Tampa, FL
Introduction: Anorectal melanoma (PAM) is a rare, aggressive neoplasm, comprising approximately 1% of anorectal malignancies and 1% of all melanoma diagnoses. Due to PAM’s location and high metastatic potential, the malignancy has a poor prognosis. Treatment remains a challenge since there is no consensus on optimal management strategy. Here we detail the clinical course of a patient diagnosed with PAM.
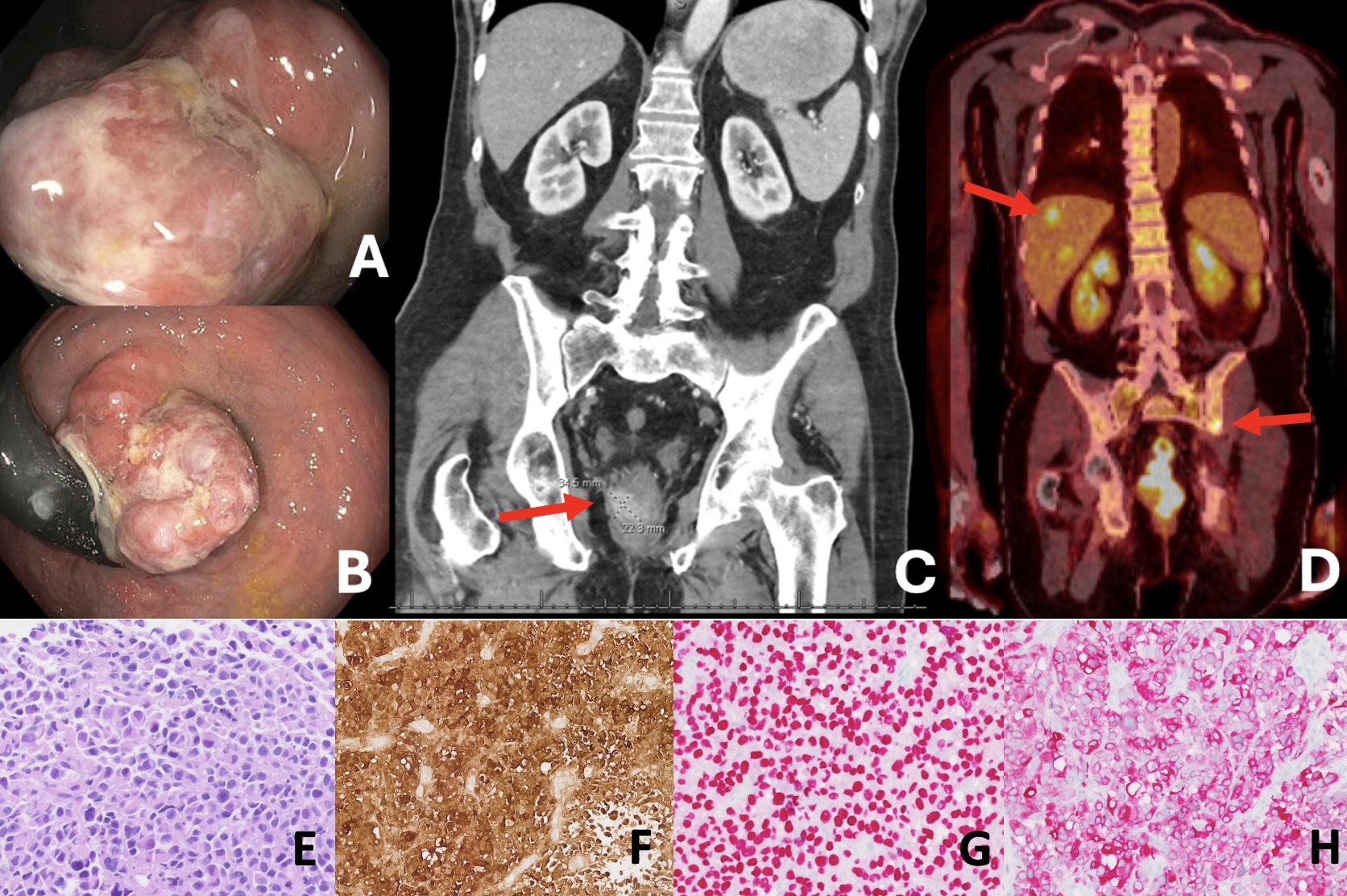
Case Description/Methods: An 87-year-old male with a history of rectal hybrid cellular angiofibroma/angiomyofibroblastoma, and cutaneous melanoma in situ of the back treated with wide local excision presented with a 4-month-history of hematochezia and worsening constipation. Exam and colonoscopy were notable for a large friable mass protruding from the anus at the dentate line. Immunohistochemistry confirmed malignant melanoma with neoplastic cells positive for S100, SOX-10, and Mart-1, and negative for pankeratin, CK7, CK20, CDX-2, P40, CK5/6, and TTF-1. PET CT further identified one FDG avid right perirectal lymph node, compatible with metastatic disease. Surgery was not pursued due to lack of survival benefit. Following treatment with three cycles of pembrolizumab, MRI identified enlargement of the tumor, extending to the internal anal sphincter, and two new suspicious mesorectal lymph nodes. Second line therapy with ipilimumab and nivolumab was initiated; after cycle 3, he unfortunately developed grade 2 immune-mediated colitis, treated with a slow steroid taper. Repeated PET CT demonstrated an interval increase in size and metabolic activity of the mass with four new right perirectal lymph nodes, various new hepatic lobe hypodensities, and new lytic lesions of multiple bones. Given clinical progression despite second-line agents, salvage therapy is being considered.
Discussion: Currently there is no clear consensus on optimal treatment regimens. Neoadjuvant immunotherapies are becoming favorable in patients with cutaneous melanoma, but notably few studies include those with mucosal melanomas. Since resection poses no survival benefit, immunotherapy was started for this patient and yet he still had disease progression after multiple lines of therapy. As evidenced in this patient, treatment of PAM remains difficult due to the aggressive nature of the malignancy and high risk of distant metastatic progression emphasizing the need for finding optimal therapies.
Disclosures:
Julia E. Gallagher, BA1, Heather Gosnell, DO2, Bharat Ponnaganti, MD1, Matthew Heckroth, MD1, Aditi Saha, MBBS1, Vita Saranga-Perry, MD3, Jeffrey A. Kooper, MD4, William Bulkeley, MD5, Jonathan Keshishian, MD5. P2476 - Skin Cancer Where the Sun Doesn’t Shine: A Rare Case of Anorectal Melanoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of South Florida, Tampa, FL; 2University of South Florida Morsani College of Medicine, Tampa, FL; 3Tampa General Hospital / University of South Florida, Tampa, FL; 4University of South Florida, James A. Haley VA Hospital, Tampa, FL; 5James A. Haley Veterans' Hospital, Tampa, FL
Introduction: Anorectal melanoma (PAM) is a rare, aggressive neoplasm, comprising approximately 1% of anorectal malignancies and 1% of all melanoma diagnoses. Due to PAM’s location and high metastatic potential, the malignancy has a poor prognosis. Treatment remains a challenge since there is no consensus on optimal management strategy. Here we detail the clinical course of a patient diagnosed with PAM.
Case Description/Methods: An 87-year-old male with a history of rectal hybrid cellular angiofibroma/angiomyofibroblastoma, and cutaneous melanoma in situ of the back treated with wide local excision presented with a 4-month-history of hematochezia and worsening constipation. Exam and colonoscopy were notable for a large friable mass protruding from the anus at the dentate line. Immunohistochemistry confirmed malignant melanoma with neoplastic cells positive for S100, SOX-10, and Mart-1, and negative for pankeratin, CK7, CK20, CDX-2, P40, CK5/6, and TTF-1. PET CT further identified one FDG avid right perirectal lymph node, compatible with metastatic disease. Surgery was not pursued due to lack of survival benefit. Following treatment with three cycles of pembrolizumab, MRI identified enlargement of the tumor, extending to the internal anal sphincter, and two new suspicious mesorectal lymph nodes. Second line therapy with ipilimumab and nivolumab was initiated; after cycle 3, he unfortunately developed grade 2 immune-mediated colitis, treated with a slow steroid taper. Repeated PET CT demonstrated an interval increase in size and metabolic activity of the mass with four new right perirectal lymph nodes, various new hepatic lobe hypodensities, and new lytic lesions of multiple bones. Given clinical progression despite second-line agents, salvage therapy is being considered.
Discussion: Currently there is no clear consensus on optimal treatment regimens. Neoadjuvant immunotherapies are becoming favorable in patients with cutaneous melanoma, but notably few studies include those with mucosal melanomas. Since resection poses no survival benefit, immunotherapy was started for this patient and yet he still had disease progression after multiple lines of therapy. As evidenced in this patient, treatment of PAM remains difficult due to the aggressive nature of the malignancy and high risk of distant metastatic progression emphasizing the need for finding optimal therapies.
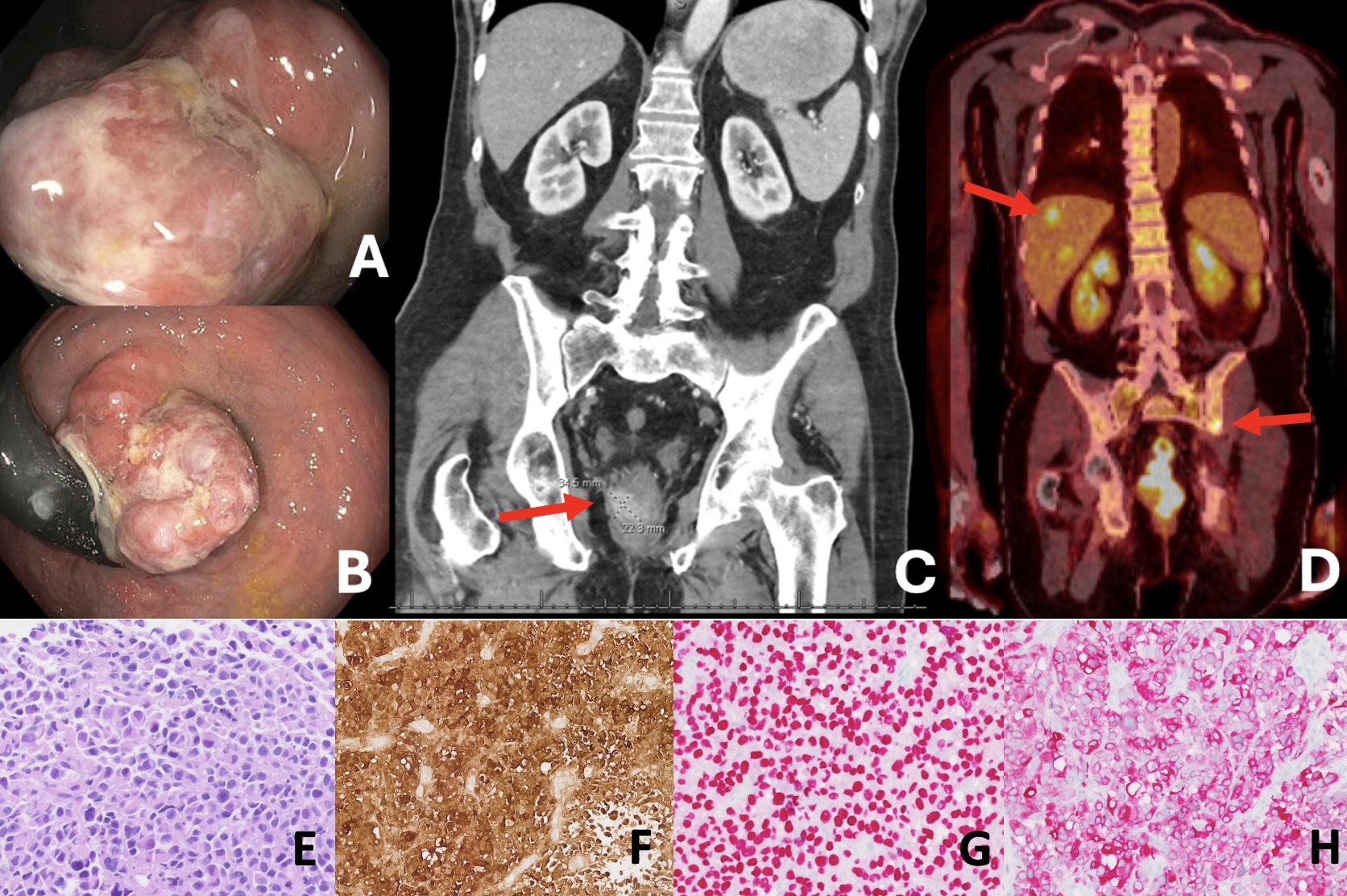
Figure: (1A-B) Images of the large rectal mass on colonoscopy with ulcerations and partial necrosis. (1C) At the time of diagnosis, initial CT Abdomen/Pelvis with contrast demonstrated the densely enhancing rectal mass, prior to immunotherapy initiation. (1D) 6 months after the initial diagnosis, PET CT following 3 cycles of pembrolizumab and 3 cycles of ipilimumab/nivolumab showed multiple new hypermetabolic lesions in the liver and bone consistent with metastases. (1E) H&E staining of the mass illustrates plasmacytoid and hyperchromatic cells lacking melanin pigment, and scattered binucleated cells with prominent nucleoli, classically seen in melanoma. (1F-H) Immunohistochemical staining positive for S100 (1F), SOX-1 (1G), MART-1 (1H) were confirmative of the diagnosis.
Disclosures:
Julia Gallagher indicated no relevant financial relationships.
Heather Gosnell indicated no relevant financial relationships.
Bharat Ponnaganti indicated no relevant financial relationships.
Matthew Heckroth indicated no relevant financial relationships.
Aditi Saha indicated no relevant financial relationships.
Vita Saranga-Perry indicated no relevant financial relationships.
Jeffrey Kooper indicated no relevant financial relationships.
William Bulkeley indicated no relevant financial relationships.
Jonathan Keshishian indicated no relevant financial relationships.
Julia E. Gallagher, BA1, Heather Gosnell, DO2, Bharat Ponnaganti, MD1, Matthew Heckroth, MD1, Aditi Saha, MBBS1, Vita Saranga-Perry, MD3, Jeffrey A. Kooper, MD4, William Bulkeley, MD5, Jonathan Keshishian, MD5. P2476 - Skin Cancer Where the Sun Doesn’t Shine: A Rare Case of Anorectal Melanoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
