Monday Poster Session
Category: GI Bleeding
P2479 - Deep Gastric Ulceration from Chronic Fentanyl and Xylazine Use
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Felicia Lee, BS
Saint Louis University School of Medicine
St. Louis, MO
Presenting Author(s)
Felicia Lee, BS1, Jay Shah, DO, MSc2, Radhika Patel, MD3, Soumojit Ghosh, MD4
1Saint Louis University School of Medicine, St. Louis, MO; 2Franciscan Health Olympia Fields, Olympia Fields, IL; 3SSM Health Saint Louis University Hospital, St. Louis, MO; 4St. Louis University, St. Louis, MO
Introduction: Xylazine is a potent central alpha-2 adrenergic agonist that was created for veterinary use. There are several case studies in Puerto Rico and Philadelphia describing the detection and effects of xylazine as a contaminant in illicit street drugs including fentanyl and heroin. Reported side effects include CNS depression, respiratory depression, and occasionally, severe skin ulcers. We describe the case of a patient who presented with hematemesis and was found to have deep gastric ulcers in the setting of chronic IV fentanyl and xylazine use.
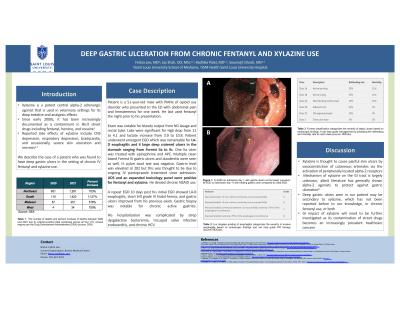
Case Description/Methods: Patient is a 51 yo male with PMHx of opioid use disorder who presented to the ED with abdominal pain and hematemesis for one week. His last fentanyl use was the night prior to his presentation. Exam was notable for bloody output from NG lavage and rectal tube. Labs were significant for Hgb drop from 11 to 4.1 and lactate increase from 3.9 to 10.8. Patient underwent emergent EGD which was remarkable for LA-D esophagitis and 4 large deep cratered ulcers in the stomach ranging from Forrest IIa to IIc. One IIa ulcer was treated with epinephrine and APC. Multiple clean based Forrest III gastric ulcers and duodenitis were seen as well. H. pylori stool test was negative. Gastrin level was elevated at 202 but this was thought to be due to ongoing IV pantoprazole treatment since admission. UDS and an expanded toxicology panel were positive for fentanyl and xylazine. He denied chronic NSAID use.
A repeat EGD 10 days post his initial EGD was done due to persistent anemia and melecna. The EGD was remarkable for LA-B esophagitis, short hill grade III hiatal hernia, and gastric ulcers improved from his previous exam. Gastric biopsy showed chronic active gastritis.
His hospitalization was complicated by strep dysgalactiae bacteremia, tricuspid valve infective endocarditis, and chronic HCV.
Discussion: Xylazine is thought to cause extensive, painful skin ulcerations by vasoconstriction of cutaneous arterioles via the activation of peripherally located alpha-2 receptors. The mechanism of xylazine on the GI tract is largely unknown, albeit literature has generally shown alpha-2 agonists to protect against gastric ulceration. The deep gastric ulcers seen in our patient may be secondary to xylazine, which has not been reported before to our knowledge, or chronic fentanyl use, or both. The gastrointestinal impact of xylazine will need to be further investigated as its contamination of street drugs becomes an increasingly prevalent healthcare concern.
Disclosures:
Felicia Lee, BS1, Jay Shah, DO, MSc2, Radhika Patel, MD3, Soumojit Ghosh, MD4. P2479 - Deep Gastric Ulceration from Chronic Fentanyl and Xylazine Use, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Saint Louis University School of Medicine, St. Louis, MO; 2Franciscan Health Olympia Fields, Olympia Fields, IL; 3SSM Health Saint Louis University Hospital, St. Louis, MO; 4St. Louis University, St. Louis, MO
Introduction: Xylazine is a potent central alpha-2 adrenergic agonist that was created for veterinary use. There are several case studies in Puerto Rico and Philadelphia describing the detection and effects of xylazine as a contaminant in illicit street drugs including fentanyl and heroin. Reported side effects include CNS depression, respiratory depression, and occasionally, severe skin ulcers. We describe the case of a patient who presented with hematemesis and was found to have deep gastric ulcers in the setting of chronic IV fentanyl and xylazine use.
Case Description/Methods: Patient is a 51 yo male with PMHx of opioid use disorder who presented to the ED with abdominal pain and hematemesis for one week. His last fentanyl use was the night prior to his presentation. Exam was notable for bloody output from NG lavage and rectal tube. Labs were significant for Hgb drop from 11 to 4.1 and lactate increase from 3.9 to 10.8. Patient underwent emergent EGD which was remarkable for LA-D esophagitis and 4 large deep cratered ulcers in the stomach ranging from Forrest IIa to IIc. One IIa ulcer was treated with epinephrine and APC. Multiple clean based Forrest III gastric ulcers and duodenitis were seen as well. H. pylori stool test was negative. Gastrin level was elevated at 202 but this was thought to be due to ongoing IV pantoprazole treatment since admission. UDS and an expanded toxicology panel were positive for fentanyl and xylazine. He denied chronic NSAID use.
A repeat EGD 10 days post his initial EGD was done due to persistent anemia and melecna. The EGD was remarkable for LA-B esophagitis, short hill grade III hiatal hernia, and gastric ulcers improved from his previous exam. Gastric biopsy showed chronic active gastritis.
His hospitalization was complicated by strep dysgalactiae bacteremia, tricuspid valve infective endocarditis, and chronic HCV.
Discussion: Xylazine is thought to cause extensive, painful skin ulcerations by vasoconstriction of cutaneous arterioles via the activation of peripherally located alpha-2 receptors. The mechanism of xylazine on the GI tract is largely unknown, albeit literature has generally shown alpha-2 agonists to protect against gastric ulceration. The deep gastric ulcers seen in our patient may be secondary to xylazine, which has not been reported before to our knowledge, or chronic fentanyl use, or both. The gastrointestinal impact of xylazine will need to be further investigated as its contamination of street drugs becomes an increasingly prevalent healthcare concern.
Disclosures:
Felicia Lee indicated no relevant financial relationships.
Jay Shah indicated no relevant financial relationships.
Radhika Patel indicated no relevant financial relationships.
Soumojit Ghosh indicated no relevant financial relationships.
Felicia Lee, BS1, Jay Shah, DO, MSc2, Radhika Patel, MD3, Soumojit Ghosh, MD4. P2479 - Deep Gastric Ulceration from Chronic Fentanyl and Xylazine Use, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
