Monday Poster Session
Category: Colorectal Cancer Prevention
P2164 - Double Trouble: Unmasking Colonic MALT Lymphoma in Two Cecal Polyps
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Iqra Kazi, MD
University of Texas Health San Antonio
San Antonio, TX
Presenting Author(s)
Iqra Kazi, MD, Colton Blinka, BS, Sarah Marucci, MD, MPH, Courtney Thomas, DO
University of Texas Health San Antonio, San Antonio, TX
Introduction: Primary colonic mucosa-associated lymphoid tissue (MALT) lymphoma is a rare type of low-grade B cell lymphoma. Patients are often asymptomatic and diagnosed on screening colonoscopy. They can also present with abdominal pain, weight loss, diarrhea, constipation, mucoid stool or hematochezia, with or without B symptoms. We present such case found on routine screening colonoscopy.
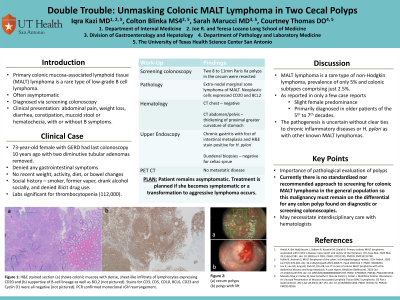
Case Description/Methods: A 73-year-old female with GERD had last colonoscopy 10 years ago with two diminutive tubular adenomas removed. She denied any gastrointestinal symptoms and no recent weight, activity, diet, or bowel changes. She is a smoker and former vaper, drank alcohol socially, and denied illicit drug use. Labs significant for thrombocytopenia (112,000). Screening colonoscopy revealed two 8 to 11mm Paris IIa polyps in the cecum which were resected. Pathology showed extranodal marginal zone lymphoma of MALT. Neoplastic cells expressed CD20 and BCL2 and lacked CD3, CD5, CD43, CD10, BCL6, CD23 and cyclin D1. Hematology evaluated for underlying etiology. CT chest was negative; CT abdomen/pelvis showed thickening of proximal greater curvature of the stomach. Upper endoscopy showed chronic gastritis with a foci of intestinal metaplasia and H&E stain positive for H. pylori. Duodenal biopsies were negative for celiac sprue. She was treated for H. pylori. PET CT showed no metastatic disease. She is currently remains asymptomatic. Treatment is planned if she becomes symptomatic or a transformation to aggressive lymphoma occurs.
Discussion: MALT lymphoma is a rare type of non-Hodgkin lymphoma with a prevalence of only 5% and colonic subtypes comprising just 2.5%. As reported in only a few case reports, has a slight female predominance and primarily diagnosed in older patients of the 5th to 7th decades. The pathogenesis is uncertain without clear ties to chronic inflammatory diseases or H. pylori as with other known MALT lymphomas. This case highlights the importance of pathological evaluation of polyps removed during colonoscopy in both symptomatic and asymptomatic patients. There is no standardized nor recommended approach to screening for colonic MALT lymphoma in the general population so this malignancy must remain on the differential for any colon polyp found on diagnostic or screening colonoscopies. Gastroenterologists should be aware of colonic manifestations of MALT lymphoma which may necessitate interdisciplinary care with hematologists to determine individualized management options for these patients.
Disclosures:
Iqra Kazi, MD, Colton Blinka, BS, Sarah Marucci, MD, MPH, Courtney Thomas, DO. P2164 - Double Trouble: Unmasking Colonic MALT Lymphoma in Two Cecal Polyps, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Texas Health San Antonio, San Antonio, TX
Introduction: Primary colonic mucosa-associated lymphoid tissue (MALT) lymphoma is a rare type of low-grade B cell lymphoma. Patients are often asymptomatic and diagnosed on screening colonoscopy. They can also present with abdominal pain, weight loss, diarrhea, constipation, mucoid stool or hematochezia, with or without B symptoms. We present such case found on routine screening colonoscopy.
Case Description/Methods: A 73-year-old female with GERD had last colonoscopy 10 years ago with two diminutive tubular adenomas removed. She denied any gastrointestinal symptoms and no recent weight, activity, diet, or bowel changes. She is a smoker and former vaper, drank alcohol socially, and denied illicit drug use. Labs significant for thrombocytopenia (112,000). Screening colonoscopy revealed two 8 to 11mm Paris IIa polyps in the cecum which were resected. Pathology showed extranodal marginal zone lymphoma of MALT. Neoplastic cells expressed CD20 and BCL2 and lacked CD3, CD5, CD43, CD10, BCL6, CD23 and cyclin D1. Hematology evaluated for underlying etiology. CT chest was negative; CT abdomen/pelvis showed thickening of proximal greater curvature of the stomach. Upper endoscopy showed chronic gastritis with a foci of intestinal metaplasia and H&E stain positive for H. pylori. Duodenal biopsies were negative for celiac sprue. She was treated for H. pylori. PET CT showed no metastatic disease. She is currently remains asymptomatic. Treatment is planned if she becomes symptomatic or a transformation to aggressive lymphoma occurs.
Discussion: MALT lymphoma is a rare type of non-Hodgkin lymphoma with a prevalence of only 5% and colonic subtypes comprising just 2.5%. As reported in only a few case reports, has a slight female predominance and primarily diagnosed in older patients of the 5th to 7th decades. The pathogenesis is uncertain without clear ties to chronic inflammatory diseases or H. pylori as with other known MALT lymphomas. This case highlights the importance of pathological evaluation of polyps removed during colonoscopy in both symptomatic and asymptomatic patients. There is no standardized nor recommended approach to screening for colonic MALT lymphoma in the general population so this malignancy must remain on the differential for any colon polyp found on diagnostic or screening colonoscopies. Gastroenterologists should be aware of colonic manifestations of MALT lymphoma which may necessitate interdisciplinary care with hematologists to determine individualized management options for these patients.
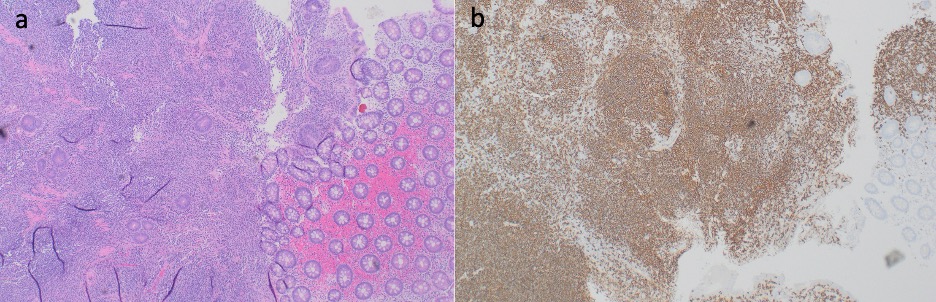
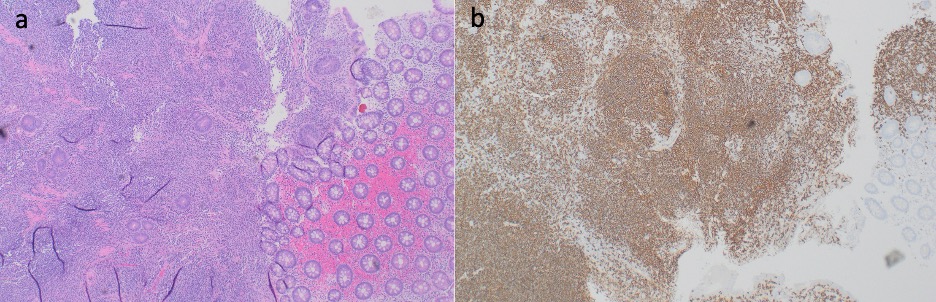
Figure: Figure 1: H&E stained section (a) shows colonic mucosa with dense, sheet-like infiltrate of lymphocytes expressing CD20 and (b) supportive of B-cell lineage as well as BCL2 (not pictured). Stains for CD3, CD5, CD10, BCL6, CD23 and Cyclin D1 were all negative (not pictured). PCR confirmed monoclonal IGH rearrangement.
Disclosures:
Iqra Kazi indicated no relevant financial relationships.
Colton Blinka indicated no relevant financial relationships.
Sarah Marucci indicated no relevant financial relationships.
Courtney Thomas indicated no relevant financial relationships.
Iqra Kazi, MD, Colton Blinka, BS, Sarah Marucci, MD, MPH, Courtney Thomas, DO. P2164 - Double Trouble: Unmasking Colonic MALT Lymphoma in Two Cecal Polyps, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
