Monday Poster Session
Category: Colon
P1993 - When Imaging Looks Like SCAD But Pathology Shows Collagenous Colitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Ethan Chambers, MS, MD
Norwalk Hospital
Fairfield, CT
Presenting Author(s)
Ethan Chambers, MS, MD1, Gurjeet Judge, MD2, Ysabel Ilagan-Ying, MD3
1Norwalk Hospital, Fairfield, CT; 2Norwalk Hospital, Norwalk, CT; 3Yale Digestive Diseases, New Haven, CT
Introduction: Segmental colitis associated with diverticulosis (SCAD) and Collagenous Colitis present with similar symptoms, making it challenging to distinguish between the two diseases based solely on imaging, labs, and clinical history. Colonoscopy and histological analysis are essential to accurately diagnose the condition and initiate appropriate treatment.
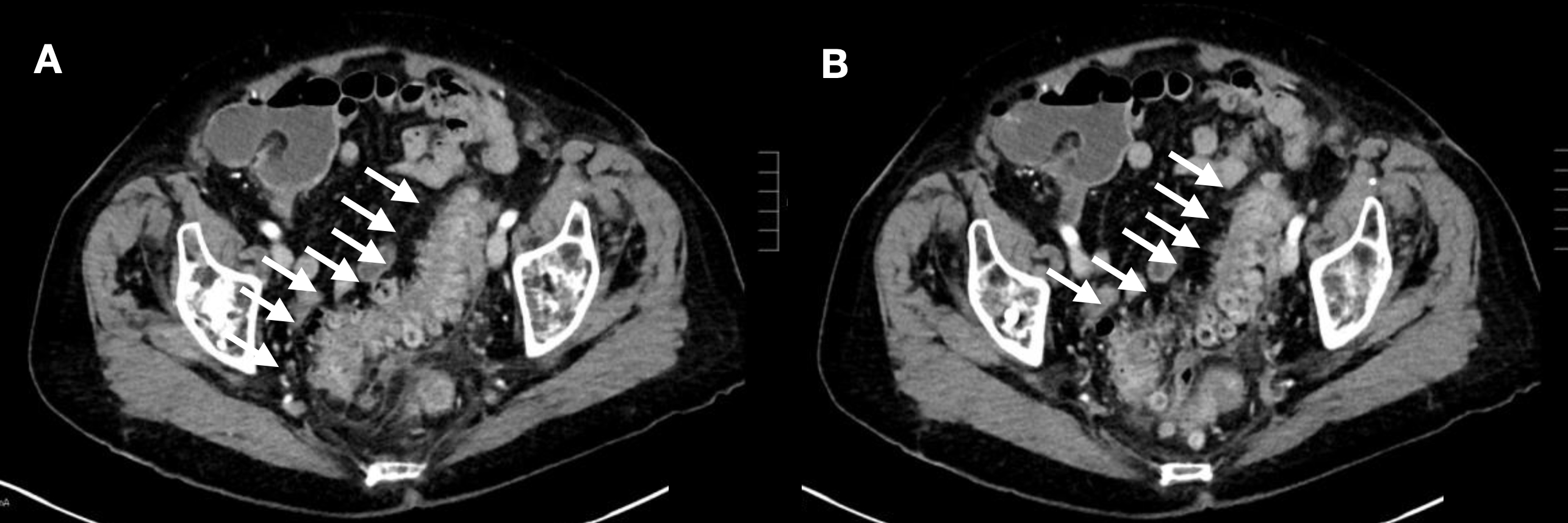
Case Description/Methods: An 88-year-old woman with a history of breast cancer and depression presented to the hospital due to one week of campy, non-bloody diarrhea for one week that did not improve with loperamide. She was hemodynamically stable upon admission, and initial CT imaging suggested SCAD. Subsequent colonoscopy revealed a benign intrinsic stricture measuring 20 cm in length in the rectosigmoid colon, along with severe diverticulosis but without signs of inflammation or masses. Biopsies were taken, and initial post-procedure recommendations included resuming a regular diet and increasing fiber intake. However, due to persistent diarrhea, she could not be discharged. Biopsy results later confirmed collagenous colitis predominantly in the right colon. Treatment with Budesonide was initiated, which quickly improved her diarrhea, and she returned to her nursing facility with close gastroenterology follow-up.
Discussion: Microscopic colitis encompasses two primary subtypes—lymphocytic and collagenous colitis—both characterized by chronic diarrhea [1]. Common symptoms include urgency of bowel movements, nocturnal stools, fecal incontinence, abdominal pain, fatigue, and weight loss [2]. Active disease is defined as more than three stools per day or more than one watery stool per day for at least one week [3]. Diagnosis relies on histological examination of biopsied tissue obtained during colonoscopy. Histological findings typical of collagenous colitis include thickening of the subepithelial collagen band, surface epithelial injury, increased lamina propria inflammation, and elevated intraepithelial lymphocytes. SCAD, on the other hand, refers to nonspecific localized inflammation in areas affected by diverticulosis and is reported in 1.2%-11.4% of patients with diverticular disease [4]. Symptoms of SCAD include chronic diarrhea, cramping, and abdominal pain. During colonoscopy, SCAD is characterized by histologically normal rectal mucosa and the presence of multiple diverticula [5]. Differential diagnosis between collagenous colitis and SCAD is primarily based on the histological examination of colonic epithelium obtained during colonoscopy.
Disclosures:
Ethan Chambers, MS, MD1, Gurjeet Judge, MD2, Ysabel Ilagan-Ying, MD3. P1993 - When Imaging Looks Like SCAD But Pathology Shows Collagenous Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Norwalk Hospital, Fairfield, CT; 2Norwalk Hospital, Norwalk, CT; 3Yale Digestive Diseases, New Haven, CT
Introduction: Segmental colitis associated with diverticulosis (SCAD) and Collagenous Colitis present with similar symptoms, making it challenging to distinguish between the two diseases based solely on imaging, labs, and clinical history. Colonoscopy and histological analysis are essential to accurately diagnose the condition and initiate appropriate treatment.
Case Description/Methods: An 88-year-old woman with a history of breast cancer and depression presented to the hospital due to one week of campy, non-bloody diarrhea for one week that did not improve with loperamide. She was hemodynamically stable upon admission, and initial CT imaging suggested SCAD. Subsequent colonoscopy revealed a benign intrinsic stricture measuring 20 cm in length in the rectosigmoid colon, along with severe diverticulosis but without signs of inflammation or masses. Biopsies were taken, and initial post-procedure recommendations included resuming a regular diet and increasing fiber intake. However, due to persistent diarrhea, she could not be discharged. Biopsy results later confirmed collagenous colitis predominantly in the right colon. Treatment with Budesonide was initiated, which quickly improved her diarrhea, and she returned to her nursing facility with close gastroenterology follow-up.
Discussion: Microscopic colitis encompasses two primary subtypes—lymphocytic and collagenous colitis—both characterized by chronic diarrhea [1]. Common symptoms include urgency of bowel movements, nocturnal stools, fecal incontinence, abdominal pain, fatigue, and weight loss [2]. Active disease is defined as more than three stools per day or more than one watery stool per day for at least one week [3]. Diagnosis relies on histological examination of biopsied tissue obtained during colonoscopy. Histological findings typical of collagenous colitis include thickening of the subepithelial collagen band, surface epithelial injury, increased lamina propria inflammation, and elevated intraepithelial lymphocytes. SCAD, on the other hand, refers to nonspecific localized inflammation in areas affected by diverticulosis and is reported in 1.2%-11.4% of patients with diverticular disease [4]. Symptoms of SCAD include chronic diarrhea, cramping, and abdominal pain. During colonoscopy, SCAD is characterized by histologically normal rectal mucosa and the presence of multiple diverticula [5]. Differential diagnosis between collagenous colitis and SCAD is primarily based on the histological examination of colonic epithelium obtained during colonoscopy.
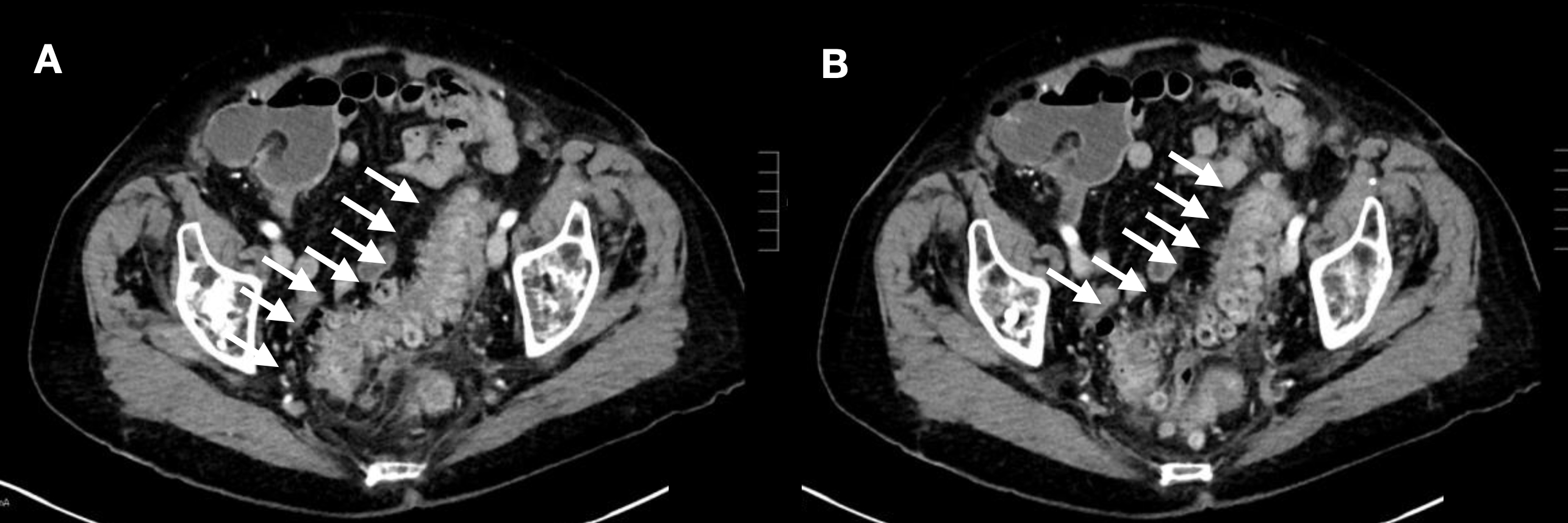
Figure: CT findings (A and B, arrows) favor acute rectosigmoid colitis or segmental colitis associated with diverticulosis (SCAD) over diverticulitis. At the junction of the descending and sigmoid colon, there is an abrupt change in luminal caliber with upstream fluid-filled large bowel.
Disclosures:
Ethan Chambers indicated no relevant financial relationships.
Gurjeet Judge indicated no relevant financial relationships.
Ysabel Ilagan-Ying indicated no relevant financial relationships.
Ethan Chambers, MS, MD1, Gurjeet Judge, MD2, Ysabel Ilagan-Ying, MD3. P1993 - When Imaging Looks Like SCAD But Pathology Shows Collagenous Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

