Monday Poster Session
Category: Colon
P1994 - Pseudomembranous Colitis: Unveiling An Infrequent Culprit Beyond Clostridium difficile - A Case Report
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Manasa Ginjupalli, MBBS, MD
The Brooklyn Hospital Center
New York, NY
Presenting Author(s)
Manasa Ginjupalli, MBBS, MD1, Jayalekshmi Jayakumar, MBBS, MD2, Hamsika Moparty, MD2, Praneeth Bandaru, MBBS, MD3, Vikash Kumar, MD4, Ali Wakil, MD3, Camelia Ciobanu, MD3, Arnold N. Forlemu, MD, MPH5, Jeeva Jaganathan, MD3, Vijay Reddy Gayam, MD6, Denzil Etienne, MD3, Madhavi Reddy, MD, FACG3
1The Brooklyn Hospital Center, New York, NY; 2The Brooklyn Hospital Center, Brooklyn, NY; 3Brooklyn Hospital Center, Brooklyn, NY; 4Creighton University School of Medicine, Brooklyn, NY; 5Brooklyn Hospital Center, Athens, GA; 6University of Texas Southwestern Medical Center, Dallas, TX
Introduction: Pseudomembranous colitis [PC] is a severe inflammatory disorder of the colon marked by yellowish white plaques coalescing to form a pseudomembrane lining the colonic wall. Historically, clostridium difficile [C. diff] infection is identified as the trigger in most cases. Less common etiologies include severe cases of ischemic colitis, collagenous colitis, inflammatory bowel disease, infections due to virus, other bacterial and parasitic organisms, Behcet’s Disease, chemotherapy or immunotherapy, and toxins. Due to rarity, these conditions are frequently overlooked posing diagnostic and therapeutic challenges. We present a case of PC, most likely because of checkpoint inhibitor (CPI) therapy.
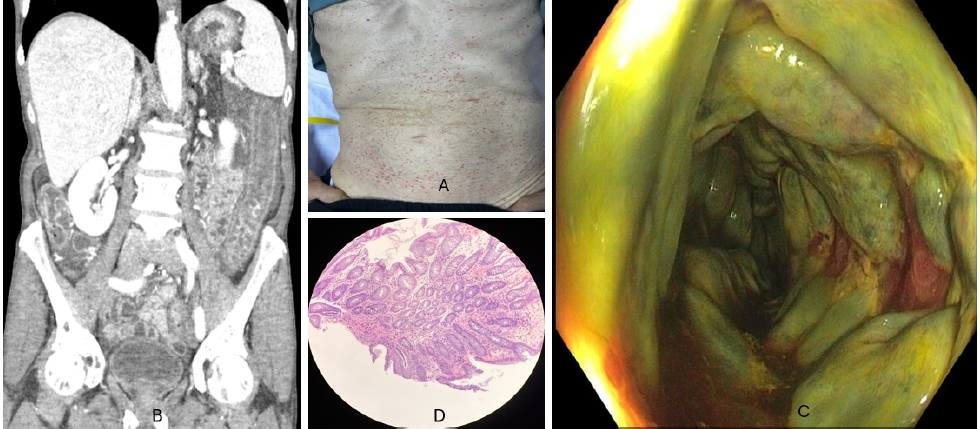
Case Description/Methods: A 68-year-old male with stage IV adenocarcinoma of gastroesophageal junction and chronic lymphocytic leukemia on Nivolumab (PD-1 inhibitor, a class of CPI) for last four months presented with abdominal pain, hematochezia and diarrhea for a day. He had normal vitals with significant physical exam findings of palpable purpura [A] and mild diffuse abdominal tenderness. Labs showed leukocytosis (41k) with absolute neutrophil count of 1000 and normal lactate. CT abdomen showed new pancolitis with mucosal thickening, any negative for significant atherosclerotic burden [B]. Flexible Sigmoidoscopy showed severe edema and circumferentially extending, confluent yellowish green exudates suggestive of pseudomembranous colitis starting from sigmoid and extending proximally [C]. C. Diff and CMV PCR sent from endoscopy lab had resulted negative. Superficial biopsies taken from the mucosa without pseudomembranous covering were unrevealing [D]. After all other common causes of PC were ruled out, provisional diagnosis of CPI/Immunotherapy-induced PC was made. A plan to start IV steroids and an oncology referral was made to discuss potential adjustments to immunotherapy.
Discussion: The occurrence of PC in patients on immunotherapy has been documented in literature primarily in association with concurrent C. diff infection. However, PC solely attributed to immunotherapy is rarely reported, with only one previous case noted with pembrolizumab used in treatment for HCC. To our knowledge, our case is the first documented instance of nivolumab-induced PC. This underscores the importance of thorough history-taking and consideration of less common etiologies of PC before presuming C. diff infection. Accurate identification of the underlying cause is crucial for targeted management and preventing recurrence.
Disclosures:
Manasa Ginjupalli, MBBS, MD1, Jayalekshmi Jayakumar, MBBS, MD2, Hamsika Moparty, MD2, Praneeth Bandaru, MBBS, MD3, Vikash Kumar, MD4, Ali Wakil, MD3, Camelia Ciobanu, MD3, Arnold N. Forlemu, MD, MPH5, Jeeva Jaganathan, MD3, Vijay Reddy Gayam, MD6, Denzil Etienne, MD3, Madhavi Reddy, MD, FACG3. P1994 - Pseudomembranous Colitis: Unveiling An Infrequent Culprit Beyond <i>Clostridium difficile</i> - A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1The Brooklyn Hospital Center, New York, NY; 2The Brooklyn Hospital Center, Brooklyn, NY; 3Brooklyn Hospital Center, Brooklyn, NY; 4Creighton University School of Medicine, Brooklyn, NY; 5Brooklyn Hospital Center, Athens, GA; 6University of Texas Southwestern Medical Center, Dallas, TX
Introduction: Pseudomembranous colitis [PC] is a severe inflammatory disorder of the colon marked by yellowish white plaques coalescing to form a pseudomembrane lining the colonic wall. Historically, clostridium difficile [C. diff] infection is identified as the trigger in most cases. Less common etiologies include severe cases of ischemic colitis, collagenous colitis, inflammatory bowel disease, infections due to virus, other bacterial and parasitic organisms, Behcet’s Disease, chemotherapy or immunotherapy, and toxins. Due to rarity, these conditions are frequently overlooked posing diagnostic and therapeutic challenges. We present a case of PC, most likely because of checkpoint inhibitor (CPI) therapy.
Case Description/Methods: A 68-year-old male with stage IV adenocarcinoma of gastroesophageal junction and chronic lymphocytic leukemia on Nivolumab (PD-1 inhibitor, a class of CPI) for last four months presented with abdominal pain, hematochezia and diarrhea for a day. He had normal vitals with significant physical exam findings of palpable purpura [A] and mild diffuse abdominal tenderness. Labs showed leukocytosis (41k) with absolute neutrophil count of 1000 and normal lactate. CT abdomen showed new pancolitis with mucosal thickening, any negative for significant atherosclerotic burden [B]. Flexible Sigmoidoscopy showed severe edema and circumferentially extending, confluent yellowish green exudates suggestive of pseudomembranous colitis starting from sigmoid and extending proximally [C]. C. Diff and CMV PCR sent from endoscopy lab had resulted negative. Superficial biopsies taken from the mucosa without pseudomembranous covering were unrevealing [D]. After all other common causes of PC were ruled out, provisional diagnosis of CPI/Immunotherapy-induced PC was made. A plan to start IV steroids and an oncology referral was made to discuss potential adjustments to immunotherapy.
Discussion: The occurrence of PC in patients on immunotherapy has been documented in literature primarily in association with concurrent C. diff infection. However, PC solely attributed to immunotherapy is rarely reported, with only one previous case noted with pembrolizumab used in treatment for HCC. To our knowledge, our case is the first documented instance of nivolumab-induced PC. This underscores the importance of thorough history-taking and consideration of less common etiologies of PC before presuming C. diff infection. Accurate identification of the underlying cause is crucial for targeted management and preventing recurrence.
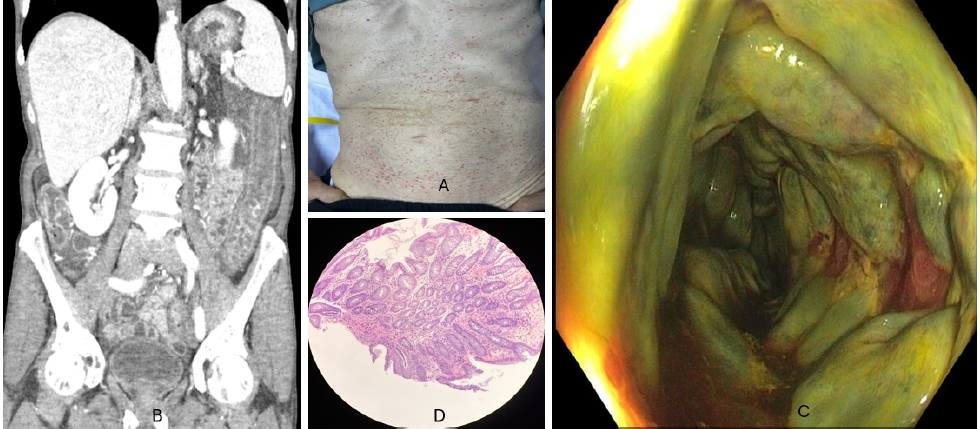
Figure: Figure 1: [A] CT Abdomen showing Pancolitis, [B] Abdominal Examination findings, [C] Endoscopic demonstration of pseudomembranes with diffuse exudates, [D] Histology of the colonic biopsy.
Disclosures:
Manasa Ginjupalli indicated no relevant financial relationships.
Jayalekshmi Jayakumar indicated no relevant financial relationships.
Hamsika Moparty indicated no relevant financial relationships.
Praneeth Bandaru indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Ali Wakil indicated no relevant financial relationships.
Camelia Ciobanu indicated no relevant financial relationships.
Arnold Forlemu indicated no relevant financial relationships.
Jeeva Jaganathan indicated no relevant financial relationships.
Vijay Reddy Gayam indicated no relevant financial relationships.
Denzil Etienne indicated no relevant financial relationships.
Madhavi Reddy indicated no relevant financial relationships.
Manasa Ginjupalli, MBBS, MD1, Jayalekshmi Jayakumar, MBBS, MD2, Hamsika Moparty, MD2, Praneeth Bandaru, MBBS, MD3, Vikash Kumar, MD4, Ali Wakil, MD3, Camelia Ciobanu, MD3, Arnold N. Forlemu, MD, MPH5, Jeeva Jaganathan, MD3, Vijay Reddy Gayam, MD6, Denzil Etienne, MD3, Madhavi Reddy, MD, FACG3. P1994 - Pseudomembranous Colitis: Unveiling An Infrequent Culprit Beyond <i>Clostridium difficile</i> - A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

