Monday Poster Session
Category: Colon
P1927 - Impact of Chemotherapy Sequence on Survival Outcomes in Colorectal Cancer Patients Undergoing Surgery: A Comprehensive Analysis of Clinical and Pathological Predictors
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- FM
Fardad Moshtagh Sisan, DO
Valley Hospital Medical Center
Porter Ranch, CA
Presenting Author(s)
Fardad Moshtagh Sisan, DO1, Elen Sarkisyan, DO2, John Ko, DO2, Heya Abid, DO2, Alice Luu, DO2, Dai-An Vo-Ba, DO2, Joseph Davis, DO3
1Valley Hospital Medical Center, Porter Ranch, CA; 2Valley Hospital Medical Center, Las Vegas, NV; 3Western University of Health Sciences, College of Osteopathic Medicine, Colton, CA
Introduction: Colorectal cancer is a common and deadly cancer globally. Standard treatment usually involves both surgery and chemotherapy, but the best sequence is still debated. Neoadjuvant chemotherapy may shrink tumors and improve outcomes, while adjuvant chemotherapy aims to eliminate residual disease.
Methods: This study examines the effects of different chemotherapy sequences on survival in colorectal adenocarcinoma using data from the Surveillance, Epidemiology, and End Results (SEER) databank. We conducted survival analysis and Cox proportional hazards modeling, evaluating factors like tumor stage, size, and primary site.
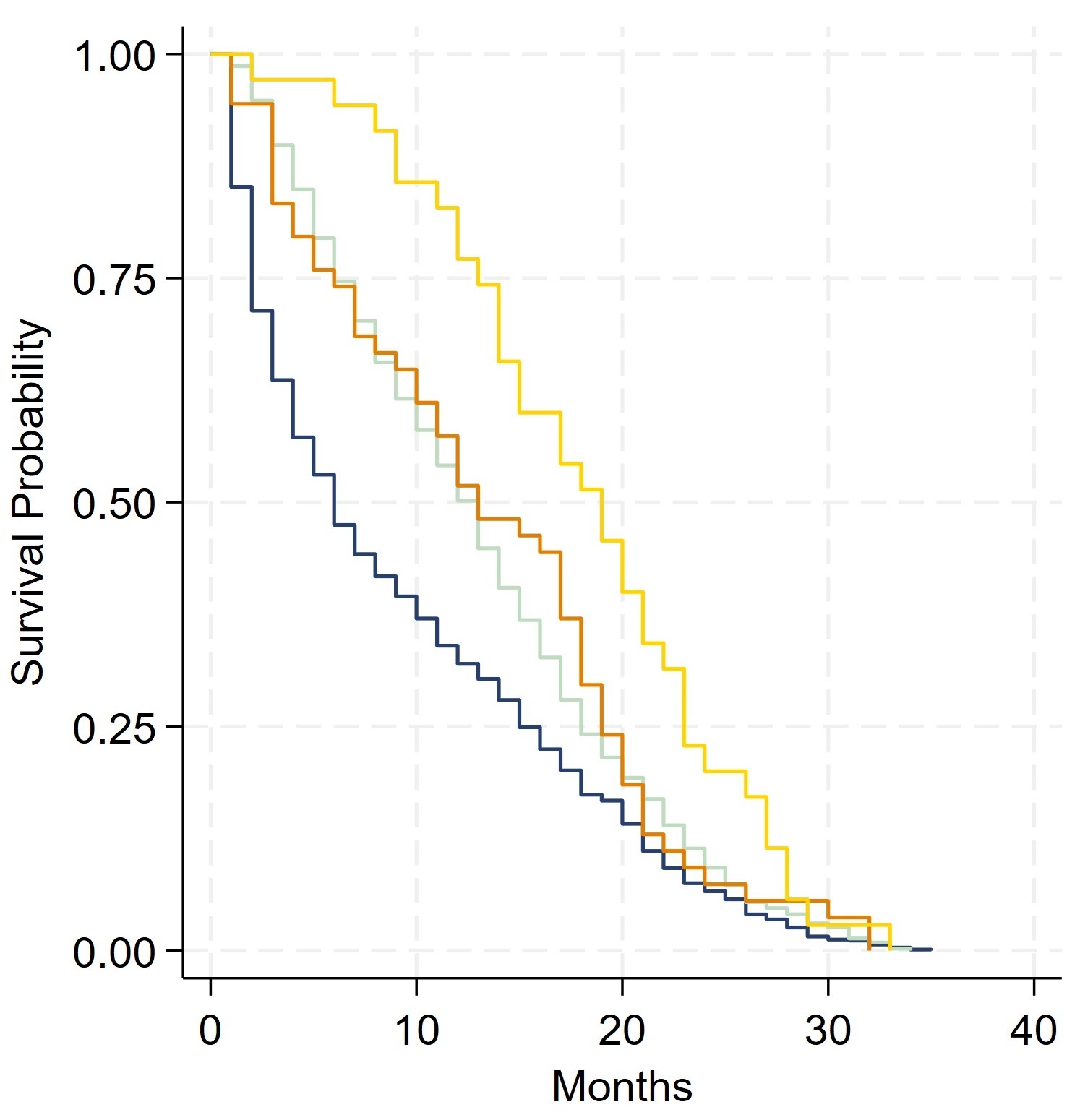
Results: The log-rank test compared survival across four groups: surgery only, chemotherapy before surgery, chemotherapy after surgery, and chemotherapy both before and after surgery. Significant differences were found among these groups (P < 0.01). Pairwise comparisons revealed no significant survival difference between chemotherapy before surgery or chemotherapy after surgery (P = 0.712). However, other pairwise comparisons showed significant differences (P < 0.01). The Cox model evaluated clinical variables on survival, including CEA levels, T stage, N stage, M stage, sex, primary tumor site, and tumor size, with chemotherapy sequence as a stratification variable. M stage, N stage, T stage, and tumor size were significant predictors of survival (P < 0.01). Only the M stage violated the proportional hazards assumption (P = 0.0397), while other variables met the assumption (P > 0.05). Variance Inflation Factor (VIF) values assessed multicollinearity among variables: T stage (1.15), N stage (1.09), tumor size (1.08), primary site (1.02), and sex (1.01), indicating no significant multicollinearity.
Discussion: Our survival analysis revealed significant differences based on the sequence of chemotherapy, highlighting how the order of chemotherapy treatments can dramatically impact patient survival. The Cox model identified M stage, N stage, T stage, and tumor size as crucial predictors of survival, emphasizing the importance of tumor characteristics in determining outcomes. Interestingly, the M stage violated the proportional hazards assumption, suggesting its impact on survival changes over time. The low VIF values confirm minimal multicollinearity among predictors, reinforcing the robustness of our model.
Disclosures:
Fardad Moshtagh Sisan, DO1, Elen Sarkisyan, DO2, John Ko, DO2, Heya Abid, DO2, Alice Luu, DO2, Dai-An Vo-Ba, DO2, Joseph Davis, DO3. P1927 - Impact of Chemotherapy Sequence on Survival Outcomes in Colorectal Cancer Patients Undergoing Surgery: A Comprehensive Analysis of Clinical and Pathological Predictors, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Valley Hospital Medical Center, Porter Ranch, CA; 2Valley Hospital Medical Center, Las Vegas, NV; 3Western University of Health Sciences, College of Osteopathic Medicine, Colton, CA
Introduction: Colorectal cancer is a common and deadly cancer globally. Standard treatment usually involves both surgery and chemotherapy, but the best sequence is still debated. Neoadjuvant chemotherapy may shrink tumors and improve outcomes, while adjuvant chemotherapy aims to eliminate residual disease.
Methods: This study examines the effects of different chemotherapy sequences on survival in colorectal adenocarcinoma using data from the Surveillance, Epidemiology, and End Results (SEER) databank. We conducted survival analysis and Cox proportional hazards modeling, evaluating factors like tumor stage, size, and primary site.
Results: The log-rank test compared survival across four groups: surgery only, chemotherapy before surgery, chemotherapy after surgery, and chemotherapy both before and after surgery. Significant differences were found among these groups (P < 0.01). Pairwise comparisons revealed no significant survival difference between chemotherapy before surgery or chemotherapy after surgery (P = 0.712). However, other pairwise comparisons showed significant differences (P < 0.01). The Cox model evaluated clinical variables on survival, including CEA levels, T stage, N stage, M stage, sex, primary tumor site, and tumor size, with chemotherapy sequence as a stratification variable. M stage, N stage, T stage, and tumor size were significant predictors of survival (P < 0.01). Only the M stage violated the proportional hazards assumption (P = 0.0397), while other variables met the assumption (P > 0.05). Variance Inflation Factor (VIF) values assessed multicollinearity among variables: T stage (1.15), N stage (1.09), tumor size (1.08), primary site (1.02), and sex (1.01), indicating no significant multicollinearity.
Discussion: Our survival analysis revealed significant differences based on the sequence of chemotherapy, highlighting how the order of chemotherapy treatments can dramatically impact patient survival. The Cox model identified M stage, N stage, T stage, and tumor size as crucial predictors of survival, emphasizing the importance of tumor characteristics in determining outcomes. Interestingly, the M stage violated the proportional hazards assumption, suggesting its impact on survival changes over time. The low VIF values confirm minimal multicollinearity among predictors, reinforcing the robustness of our model.
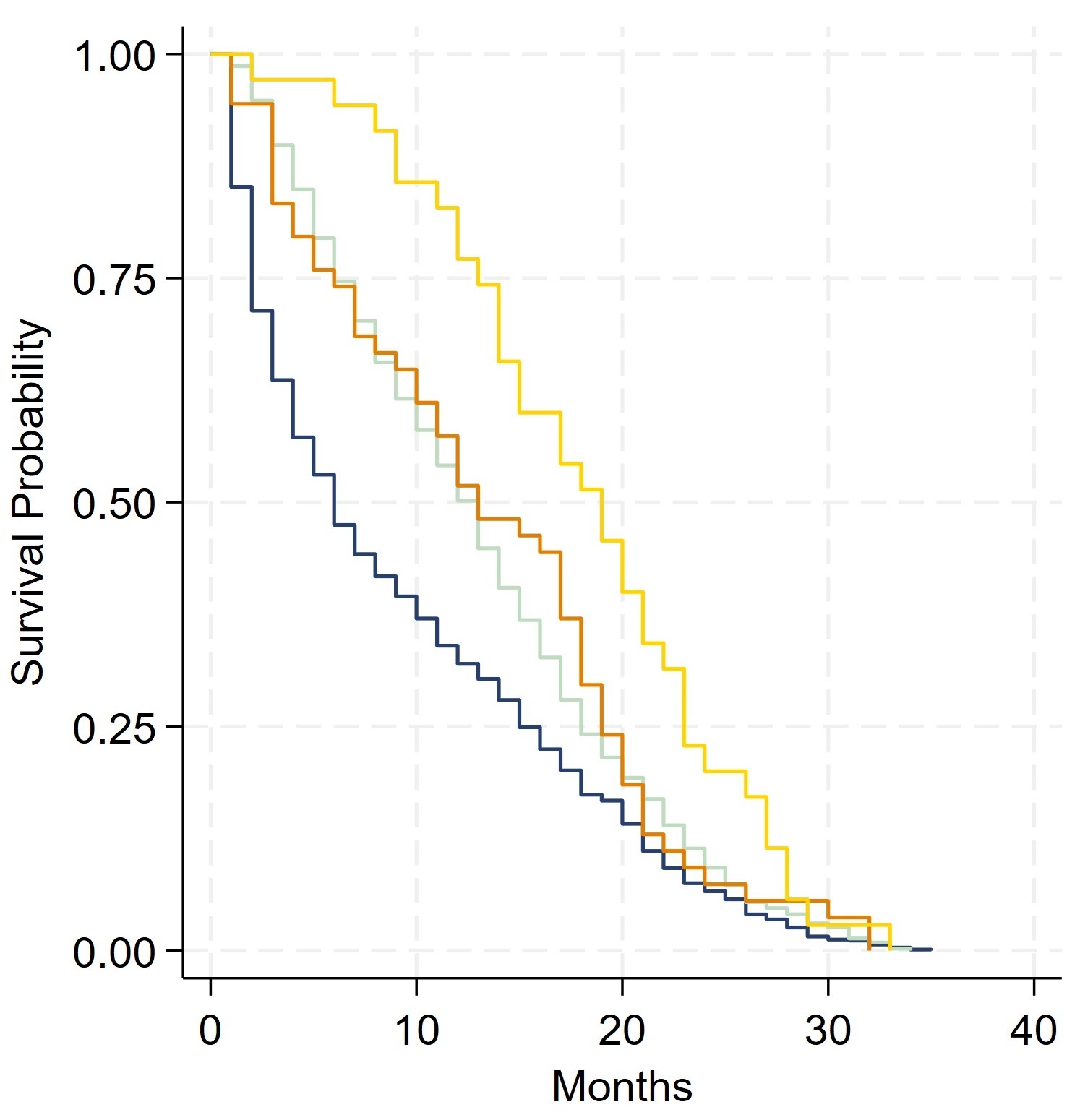
Figure: Kaplan-Meier Survival.
Blue - Surgery Only.
Light Green - Chemotherapy After Surgery.
Orange - Chemotherapy Before Surgery.
Yellow - Chemotherapy Before and After Surgery.
Blue - Surgery Only.
Light Green - Chemotherapy After Surgery.
Orange - Chemotherapy Before Surgery.
Yellow - Chemotherapy Before and After Surgery.
Disclosures:
Fardad Moshtagh Sisan indicated no relevant financial relationships.
Elen Sarkisyan indicated no relevant financial relationships.
John Ko indicated no relevant financial relationships.
Heya Abid indicated no relevant financial relationships.
Alice Luu indicated no relevant financial relationships.
Dai-An Vo-Ba indicated no relevant financial relationships.
Joseph Davis indicated no relevant financial relationships.
Fardad Moshtagh Sisan, DO1, Elen Sarkisyan, DO2, John Ko, DO2, Heya Abid, DO2, Alice Luu, DO2, Dai-An Vo-Ba, DO2, Joseph Davis, DO3. P1927 - Impact of Chemotherapy Sequence on Survival Outcomes in Colorectal Cancer Patients Undergoing Surgery: A Comprehensive Analysis of Clinical and Pathological Predictors, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
