Monday Poster Session
Category: Biliary/Pancreas
P1804 - Pancreatic Pseudoaneurysm-Induced Hemosuccus Pancreaticus: Successful Multidisciplinary Intervention
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Sushrut Ingawale, MD, MBBS
Quinnipiac University Frank H. Netter MD School of Medicine / St. Vincent's Medical Center
Bridgeport, CT
Presenting Author(s)
Sushrut Ingawale, MD, MBBS1, Pujitha Vallivedu Chennakesavulu, MD, MBBS1, Aishwarya Thakurdesai, MBBS2, Asim Haider, MD1, Mariam Farhan, MD1, Prabin Sharma, MD1
1Quinnipiac University Frank H. Netter MD School of Medicine / St. Vincent's Medical Center, Bridgeport, CT; 2University of Louisville School of Medicine, Louisville, KY
Introduction: Hemosuccus pancreaticus (HP) is a rare cause of upper gastrointestinal (GI) hemorrhage, that can result from the rupture of a pancreatic pseudoaneurysm into the pancreatic duct and is often associated with pancreatitis or pancreatic neoplasms. Here we report a case of HP presenting with abdominal pain and melena diagnosed during upper GI endoscopy (UGIE) noted to have bleeding from the ampulla of Vater into the duodenum, likely secondary to a ruptured pseudoaneurysm. This case underscores the diagnostic and therapeutic challenges necessitating multidisciplinary collaboration.
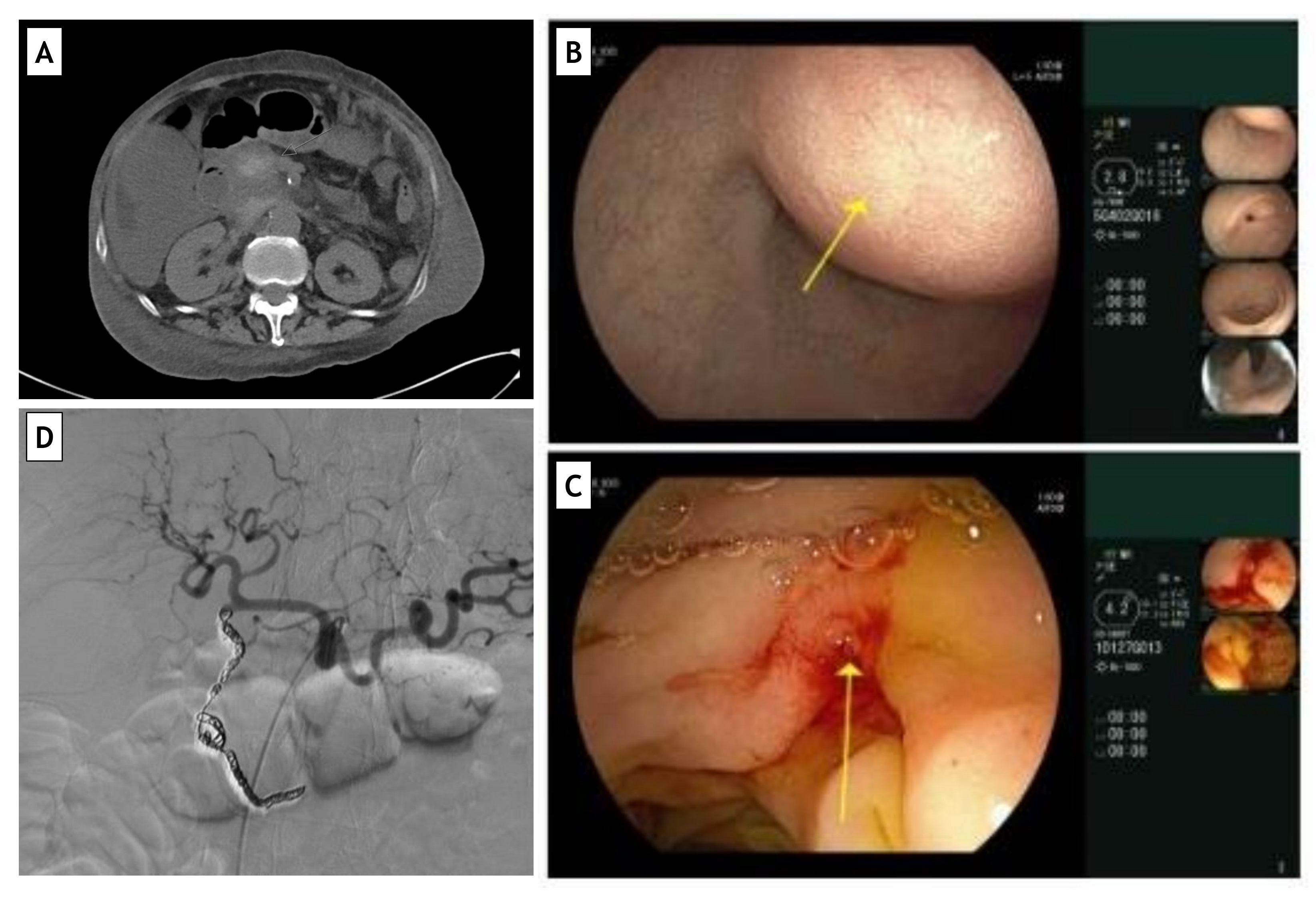
Case Description/Methods: We present a 63-year-old female with a history of hypertension, chronic kidney disease, alcohol abuse disorder, and deep venous thrombosis not on anticoagulation status post inferior vena cava filter, who presented with hematemesis and melena. Work-up revealed normocytic anemia (hemoglobin: 5.8 g/dL), normal lipase and liver function tests. A contrast CT of the abdomen (Figure) identified a heterogeneous lesion in the pancreatic head with focal enhancement, suggesting a pseudoaneurysm with hemorrhage. Additional lesions noted in the pancreatic head and tail suggested possible malignancy or chronic pancreatitis. UGIE revealed active bleeding from the ampulla of Vater. Angiography demonstrated pseudoaneurysms in the gastroduodenal artery (GDA) and inferior pancreaticoduodenal artery (IPDA). Retrograde coil embolization was performed. A follow-up CT confirmed resolution of the pseudoaneurysm and stable hematoma.
Discussion: HP presents diagnostic challenges due to its rarity and variable presentation. Diagnosis relies on clinical suspicion, imaging, and endoscopy. Intermittent bleeding can delay diagnosis, necessitating high suspicion. Contrast-enhanced CT is the gold standard for diagnosis. UGIE and Endoscopic Ultrasound (EUS) help affirm the diagnosis, while CT with contrast helps characaterize the pneudoaneurysm. Angiographic embolization has emerged as a first-line intervention for effective hemostasis while preserving pancreatic function. Surgical options are reserved for refractory cases. A multidisciplinary approach involving internal medicine, gastroenterology, interventional radiology, and surgery is crucial. Long-term surveillance is essential to monitor for recurrence, complications, or underlying pancreatic pathologies. Further research is needed to elucidate underlying mechanisms, refine treatments, and establish guidelines for managing HP, especially in atypical or refractory cases.
Disclosures:
Sushrut Ingawale, MD, MBBS1, Pujitha Vallivedu Chennakesavulu, MD, MBBS1, Aishwarya Thakurdesai, MBBS2, Asim Haider, MD1, Mariam Farhan, MD1, Prabin Sharma, MD1. P1804 - Pancreatic Pseudoaneurysm-Induced Hemosuccus Pancreaticus: Successful Multidisciplinary Intervention, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Quinnipiac University Frank H. Netter MD School of Medicine / St. Vincent's Medical Center, Bridgeport, CT; 2University of Louisville School of Medicine, Louisville, KY
Introduction: Hemosuccus pancreaticus (HP) is a rare cause of upper gastrointestinal (GI) hemorrhage, that can result from the rupture of a pancreatic pseudoaneurysm into the pancreatic duct and is often associated with pancreatitis or pancreatic neoplasms. Here we report a case of HP presenting with abdominal pain and melena diagnosed during upper GI endoscopy (UGIE) noted to have bleeding from the ampulla of Vater into the duodenum, likely secondary to a ruptured pseudoaneurysm. This case underscores the diagnostic and therapeutic challenges necessitating multidisciplinary collaboration.
Case Description/Methods: We present a 63-year-old female with a history of hypertension, chronic kidney disease, alcohol abuse disorder, and deep venous thrombosis not on anticoagulation status post inferior vena cava filter, who presented with hematemesis and melena. Work-up revealed normocytic anemia (hemoglobin: 5.8 g/dL), normal lipase and liver function tests. A contrast CT of the abdomen (Figure) identified a heterogeneous lesion in the pancreatic head with focal enhancement, suggesting a pseudoaneurysm with hemorrhage. Additional lesions noted in the pancreatic head and tail suggested possible malignancy or chronic pancreatitis. UGIE revealed active bleeding from the ampulla of Vater. Angiography demonstrated pseudoaneurysms in the gastroduodenal artery (GDA) and inferior pancreaticoduodenal artery (IPDA). Retrograde coil embolization was performed. A follow-up CT confirmed resolution of the pseudoaneurysm and stable hematoma.
Discussion: HP presents diagnostic challenges due to its rarity and variable presentation. Diagnosis relies on clinical suspicion, imaging, and endoscopy. Intermittent bleeding can delay diagnosis, necessitating high suspicion. Contrast-enhanced CT is the gold standard for diagnosis. UGIE and Endoscopic Ultrasound (EUS) help affirm the diagnosis, while CT with contrast helps characaterize the pneudoaneurysm. Angiographic embolization has emerged as a first-line intervention for effective hemostasis while preserving pancreatic function. Surgical options are reserved for refractory cases. A multidisciplinary approach involving internal medicine, gastroenterology, interventional radiology, and surgery is crucial. Long-term surveillance is essential to monitor for recurrence, complications, or underlying pancreatic pathologies. Further research is needed to elucidate underlying mechanisms, refine treatments, and establish guidelines for managing HP, especially in atypical or refractory cases.
Figure: (A) Computed Tomography Scan of Abdomen and Pelvis identifying multiple pancreatic lesions; (B) Upper GI Endoscopy (UGIE) revealing ‘subepithelial’ prominence in the duodenal bulb likely from pancreatic pseudoaneurysm; (C) Upper GI Endoscopy (UGIE) revealing ‘Hemosuccus Pancreaticus’ - active bleeding from the ampulla of Vater; and, (D) Minimally invasive therapeutic approach with favorable outcome - Post Angiographic Retrograde Coil Embolization of culprit blood vessels.
Disclosures:
Sushrut Ingawale indicated no relevant financial relationships.
Pujitha Vallivedu Chennakesavulu indicated no relevant financial relationships.
Aishwarya Thakurdesai indicated no relevant financial relationships.
Asim Haider indicated no relevant financial relationships.
Mariam Farhan indicated no relevant financial relationships.
Prabin Sharma indicated no relevant financial relationships.
Sushrut Ingawale, MD, MBBS1, Pujitha Vallivedu Chennakesavulu, MD, MBBS1, Aishwarya Thakurdesai, MBBS2, Asim Haider, MD1, Mariam Farhan, MD1, Prabin Sharma, MD1. P1804 - Pancreatic Pseudoaneurysm-Induced Hemosuccus Pancreaticus: Successful Multidisciplinary Intervention, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
