Monday Poster Session
Category: Biliary/Pancreas
P1726 - Temporal Trends and Regional Differences in Septicemia-Related Mortality in Patients With Acute Pancreatitis: A Two-Decade Analysis From 1999-2020
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ahmad Zain, MD
UChealth Parkview Medical Center
Pueblo, CO
Presenting Author(s)
Obaid Ur Rehman, MBBS1, Ahmad Zain, MD2, Fatima Ashfaq, MBBS3, Zain A. Nadeem, MBBS4, Eeshal fatima, MBBS1, Ariba Khan, MBBS1, Hammad Qadri, DO5
1Services Institute of Medical Sciences, Lahore, Punjab, Pakistan; 2UChealth Parkview Medical Center, Pueblo, CO; 3Nishtar Medical University, Lahore, Punjab, Pakistan; 4Allama Iqbal Medical College, Lahore, Punjab, Pakistan; 5United Health Services, Wilson Medical Center, Binghamton, NY
Introduction: Although acute pancreatitis is a common gastrointestinal illness with the potential to be fatal, many countries lack data on the disease burden. In 2019, 2,814,972 cases of acute pancreatitis were reported globally. This study aims to identify the temporal trends and regional variations in septicemia-related mortality in patients with acute pancreatitis in the United States, stratified by age, sex, race, and age groups.
Methods: The CDC-WONDER database was queried for data from death certificates of adults aged ≥25 years. We calculated crude mortality rates (CRs) and age-adjusted mortality rates (AAMRs) per 100,000 population. The temporal variations were delineated by estimating the annual percent change (APC) and the average annual percent change (AAPC) using Joinpoint regression.
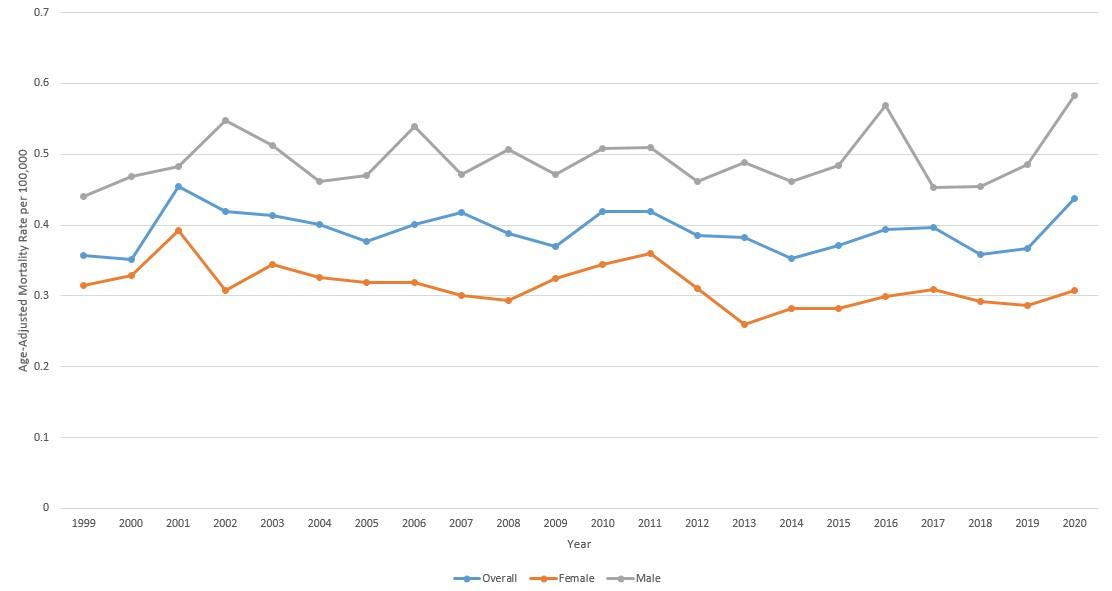
Results: From 1999 to 2020, a total of 14,757 deaths were associated with acute pancreatitis and septicemia with AAMR 0.391, (95% CI 0.385 – 0.398). The overall AAMR decreased from 1999 to 2020 (APC -0.1375, 95% CI -0.759 to 0.564). Males displayed a higher AAMR (0.475, 95% CI 0.465 – 0.486) than females (0.313, 95% CI 0.305 – 0.321). The highest AAMRs were displayed by Non-Hispanic Black or African American (0.520, 95% CI 0.422 – 0.617). Non-Hispanic white has more AAMR (0.437, 95% CI 0.401 – 0.474)
as compared to Hispanic white with (0.431, 95% CI 0.405 – 0.456).
The south had the highest AAMR (0.463, 95% CI 0.451 – 0.474), followed by the Northeast (0.377, 95% CI 0.363 – 0.392). AAMRs were noted in the West (0.370, 95% CI 0.356 – 0.383) and the Midwest (0.361, 95% CI 0.347 – 0.374). States with the most elevated AAMRs included Oklahoma, Tennessee, South Carolina, Rhode Island, and Mississippi. Minnesota, Hawaii, and Oregon have the lowest AAMR.
Rural regions showed a higher AAMR (0.446, 95% CI 0.429–0.462) than urban regions (0.388, 95% CI 0.381 – 0.395). Adults aged more than 85 years showed the greatest AAMR (CR 1.689, 95% CI 1.615 – 1.762) followed by 75-84 years (CR 1.083, 95% CI 1.045 – 1.120). 15-24 years shows least AAMR (CR 0.01, 95% CI 0.01 – 0.02).
Discussion: Our findings indicate that the mortality from septicemia-related acute pancreatitis began to rise. There is a higher mortality rate among males, non-Hispanic Black or African American, those living in rural areas and southern states, as well as those over the age of 85. To address these disparities, a targeted approach must be taken to lower the death rate among high-risk groups through the implementation of targeted measures.
Disclosures:
Obaid Ur Rehman, MBBS1, Ahmad Zain, MD2, Fatima Ashfaq, MBBS3, Zain A. Nadeem, MBBS4, Eeshal fatima, MBBS1, Ariba Khan, MBBS1, Hammad Qadri, DO5. P1726 - Temporal Trends and Regional Differences in Septicemia-Related Mortality in Patients With Acute Pancreatitis: A Two-Decade Analysis From 1999-2020, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Services Institute of Medical Sciences, Lahore, Punjab, Pakistan; 2UChealth Parkview Medical Center, Pueblo, CO; 3Nishtar Medical University, Lahore, Punjab, Pakistan; 4Allama Iqbal Medical College, Lahore, Punjab, Pakistan; 5United Health Services, Wilson Medical Center, Binghamton, NY
Introduction: Although acute pancreatitis is a common gastrointestinal illness with the potential to be fatal, many countries lack data on the disease burden. In 2019, 2,814,972 cases of acute pancreatitis were reported globally. This study aims to identify the temporal trends and regional variations in septicemia-related mortality in patients with acute pancreatitis in the United States, stratified by age, sex, race, and age groups.
Methods: The CDC-WONDER database was queried for data from death certificates of adults aged ≥25 years. We calculated crude mortality rates (CRs) and age-adjusted mortality rates (AAMRs) per 100,000 population. The temporal variations were delineated by estimating the annual percent change (APC) and the average annual percent change (AAPC) using Joinpoint regression.
Results: From 1999 to 2020, a total of 14,757 deaths were associated with acute pancreatitis and septicemia with AAMR 0.391, (95% CI 0.385 – 0.398). The overall AAMR decreased from 1999 to 2020 (APC -0.1375, 95% CI -0.759 to 0.564). Males displayed a higher AAMR (0.475, 95% CI 0.465 – 0.486) than females (0.313, 95% CI 0.305 – 0.321). The highest AAMRs were displayed by Non-Hispanic Black or African American (0.520, 95% CI 0.422 – 0.617). Non-Hispanic white has more AAMR (0.437, 95% CI 0.401 – 0.474)
as compared to Hispanic white with (0.431, 95% CI 0.405 – 0.456).
The south had the highest AAMR (0.463, 95% CI 0.451 – 0.474), followed by the Northeast (0.377, 95% CI 0.363 – 0.392). AAMRs were noted in the West (0.370, 95% CI 0.356 – 0.383) and the Midwest (0.361, 95% CI 0.347 – 0.374). States with the most elevated AAMRs included Oklahoma, Tennessee, South Carolina, Rhode Island, and Mississippi. Minnesota, Hawaii, and Oregon have the lowest AAMR.
Rural regions showed a higher AAMR (0.446, 95% CI 0.429–0.462) than urban regions (0.388, 95% CI 0.381 – 0.395). Adults aged more than 85 years showed the greatest AAMR (CR 1.689, 95% CI 1.615 – 1.762) followed by 75-84 years (CR 1.083, 95% CI 1.045 – 1.120). 15-24 years shows least AAMR (CR 0.01, 95% CI 0.01 – 0.02).
Discussion: Our findings indicate that the mortality from septicemia-related acute pancreatitis began to rise. There is a higher mortality rate among males, non-Hispanic Black or African American, those living in rural areas and southern states, as well as those over the age of 85. To address these disparities, a targeted approach must be taken to lower the death rate among high-risk groups through the implementation of targeted measures.
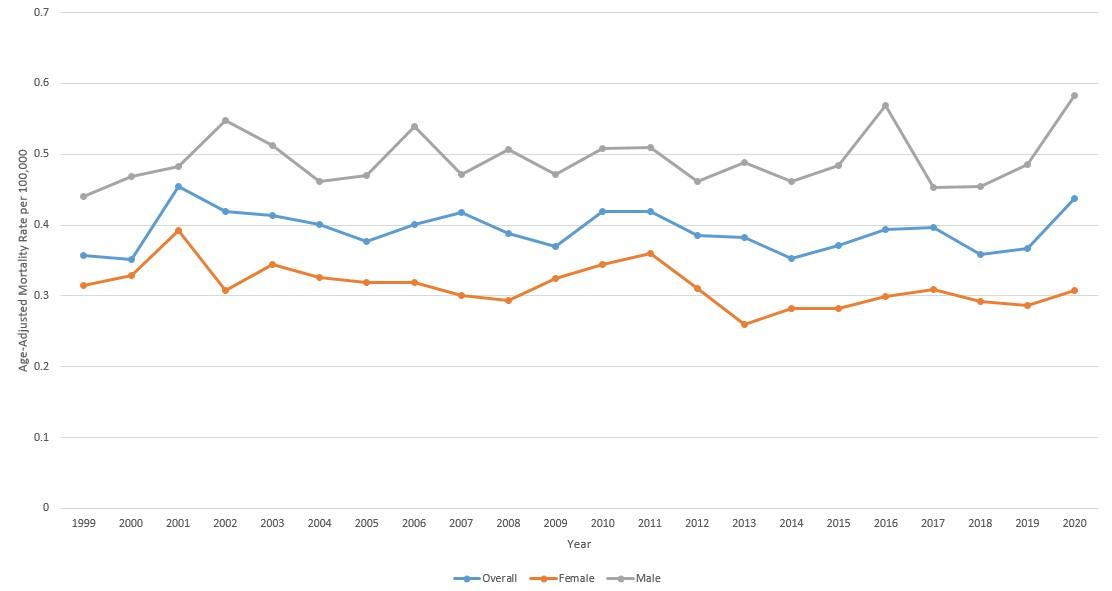
Figure:
Figure 1: Overall AAMRs of septicemia with acute pancreatitis with per 100,000 among different genders in the USA, 1999 to 2020
Figure 1: Overall AAMRs of septicemia with acute pancreatitis with per 100,000 among different genders in the USA, 1999 to 2020
Disclosures:
Obaid Ur Rehman indicated no relevant financial relationships.
Ahmad Zain indicated no relevant financial relationships.
Fatima Ashfaq indicated no relevant financial relationships.
Zain Nadeem indicated no relevant financial relationships.
Eeshal fatima indicated no relevant financial relationships.
Ariba Khan indicated no relevant financial relationships.
Hammad Qadri indicated no relevant financial relationships.
Obaid Ur Rehman, MBBS1, Ahmad Zain, MD2, Fatima Ashfaq, MBBS3, Zain A. Nadeem, MBBS4, Eeshal fatima, MBBS1, Ariba Khan, MBBS1, Hammad Qadri, DO5. P1726 - Temporal Trends and Regional Differences in Septicemia-Related Mortality in Patients With Acute Pancreatitis: A Two-Decade Analysis From 1999-2020, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
