Sunday Poster Session
Category: Biliary/Pancreas
P0033 - PSC-IBD Cohorts Show Decreased Incidence of ERCP-Associated Adverse Events Compared to Isolated PSC
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Ryan Plunkett, MD
Saint Louis University School of Medicine
St. Louis, MO
Presenting Author(s)
Ryan Plunkett, MD1, Ameya Deshmukh, DO1, Hayden Rotramel, MD2, Timothy Chrusciel, MPH3, Neel Matiwala, BS1, Rohan Tripathi, BS1, Shreeya Thussu, BS1, Jered Schenk, MD4, Antonio R. Cheesman, MD2
1Saint Louis University School of Medicine, St. Louis, MO; 2SSM Health Saint Louis University Hospital, St. Louis, MO; 3Saint Louis University, St. Louis, MO; 4Medical University of South Carolina, Charleston, SC
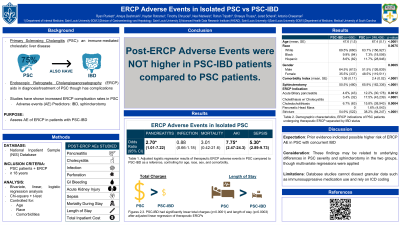
Introduction: Primary sclerosing cholangitis (PSC) is an immune-mediated, cholestatic liver disease that often coexists with Inflammatory Bowel Disease (IBD). Endoscopic Retrograde Cholangiopancreatography (ERCP) is a valuable tool in the diagnosis and treatment of PSC, though it carries risk for complications. The purpose of this study was to assess if rates of ERCP adverse events (AEs) were higher in PSC patients with IBD.
Methods: Using the National Inpatient Sample (NIS) database, PSC patients 18 years or older undergoing ERCP were identified from 2008-2019 and then organized by procedural indication, therapeutic ERCP, and sphincterotomy. Patient characteristics were found using ICD-9 and ICD-10 codes. The AEs of interest were pancreatitis, cholecystitis, infection, perforation, bleeding, acute kidney injury (AKI), sepsis, mortality, length of stay (LOS), and total charges. These were analyzed using multivariate logistic or linear regression controlling for age, race, and comorbidities. Bivariate analyses were conducted using chi-square and t-tests. Analyses accounted for the complex sampling scheme of the NIS.
Results: 284,775 PSC patients were identified as having undergone ERCP, with 0.4% (n=1,243) carrying a diagnosis of IBD. Within those undergoing therapeutic ERCP, IBD patients were more likely to have strictures (54.9% vs 38.2%, p< 0.0001), less likely to have cholelithiasis with cholecystitis (3.4% vs 17.5%, p< 0.0001) and choledocholithiasis (6.7% vs 15.8%, p=0.0004), less likely to have sphincterotomy (50.5% vs 65.9%, p< 0.0001), had a lower comorbidity index (1.05 vs 2.40, p< 0.0001), and were younger (47.6 vs 67.4 years, p< 0.0001).
After adjusted logistic regression, patients with IBD were less likely to experience the adverse events of pancreatitis (OR 2.87; 95% CI 1.19-6.92), AKI (OR 9.79; 95% CI 3.12-30.69), and sepsis (OR 7.20; 95% CI 3.92-13.23). Adjusted linear regression showed patients with IBD had shorter LOS (p< 0.0001) and lower cost (p< 0.0001).
Discussion: This NIS study reveals significantly lower rates of post-ERCP complications in PSC patients with IBD which can help guide risk assessment in that population. Notably, while there were significant differences regarding procedural indication between the two groups, these variables were controlled for in the adjusted logistic regression.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ryan Plunkett, MD1, Ameya Deshmukh, DO1, Hayden Rotramel, MD2, Timothy Chrusciel, MPH3, Neel Matiwala, BS1, Rohan Tripathi, BS1, Shreeya Thussu, BS1, Jered Schenk, MD4, Antonio R. Cheesman, MD2. P0033 - PSC-IBD Cohorts Show Decreased Incidence of ERCP-Associated Adverse Events Compared to Isolated PSC, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Saint Louis University School of Medicine, St. Louis, MO; 2SSM Health Saint Louis University Hospital, St. Louis, MO; 3Saint Louis University, St. Louis, MO; 4Medical University of South Carolina, Charleston, SC
Introduction: Primary sclerosing cholangitis (PSC) is an immune-mediated, cholestatic liver disease that often coexists with Inflammatory Bowel Disease (IBD). Endoscopic Retrograde Cholangiopancreatography (ERCP) is a valuable tool in the diagnosis and treatment of PSC, though it carries risk for complications. The purpose of this study was to assess if rates of ERCP adverse events (AEs) were higher in PSC patients with IBD.
Methods: Using the National Inpatient Sample (NIS) database, PSC patients 18 years or older undergoing ERCP were identified from 2008-2019 and then organized by procedural indication, therapeutic ERCP, and sphincterotomy. Patient characteristics were found using ICD-9 and ICD-10 codes. The AEs of interest were pancreatitis, cholecystitis, infection, perforation, bleeding, acute kidney injury (AKI), sepsis, mortality, length of stay (LOS), and total charges. These were analyzed using multivariate logistic or linear regression controlling for age, race, and comorbidities. Bivariate analyses were conducted using chi-square and t-tests. Analyses accounted for the complex sampling scheme of the NIS.
Results: 284,775 PSC patients were identified as having undergone ERCP, with 0.4% (n=1,243) carrying a diagnosis of IBD. Within those undergoing therapeutic ERCP, IBD patients were more likely to have strictures (54.9% vs 38.2%, p< 0.0001), less likely to have cholelithiasis with cholecystitis (3.4% vs 17.5%, p< 0.0001) and choledocholithiasis (6.7% vs 15.8%, p=0.0004), less likely to have sphincterotomy (50.5% vs 65.9%, p< 0.0001), had a lower comorbidity index (1.05 vs 2.40, p< 0.0001), and were younger (47.6 vs 67.4 years, p< 0.0001).
After adjusted logistic regression, patients with IBD were less likely to experience the adverse events of pancreatitis (OR 2.87; 95% CI 1.19-6.92), AKI (OR 9.79; 95% CI 3.12-30.69), and sepsis (OR 7.20; 95% CI 3.92-13.23). Adjusted linear regression showed patients with IBD had shorter LOS (p< 0.0001) and lower cost (p< 0.0001).
Discussion: This NIS study reveals significantly lower rates of post-ERCP complications in PSC patients with IBD which can help guide risk assessment in that population. Notably, while there were significant differences regarding procedural indication between the two groups, these variables were controlled for in the adjusted logistic regression.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ryan Plunkett indicated no relevant financial relationships.
Ameya Deshmukh indicated no relevant financial relationships.
Hayden Rotramel indicated no relevant financial relationships.
Timothy Chrusciel indicated no relevant financial relationships.
Neel Matiwala indicated no relevant financial relationships.
Rohan Tripathi indicated no relevant financial relationships.
Shreeya Thussu indicated no relevant financial relationships.
Jered Schenk indicated no relevant financial relationships.
Antonio Cheesman indicated no relevant financial relationships.
Ryan Plunkett, MD1, Ameya Deshmukh, DO1, Hayden Rotramel, MD2, Timothy Chrusciel, MPH3, Neel Matiwala, BS1, Rohan Tripathi, BS1, Shreeya Thussu, BS1, Jered Schenk, MD4, Antonio R. Cheesman, MD2. P0033 - PSC-IBD Cohorts Show Decreased Incidence of ERCP-Associated Adverse Events Compared to Isolated PSC, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
