Sunday Poster Session
Category: Biliary/Pancreas
P0044 - The Impact of Frailty on the Clinical Outcomes of Acute Cholangitis: A Retrospective Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Ali Jaan, MD
Rochester General Hospital
Rochester, NY
Presenting Author(s)
Ali Jaan, MD1, Umer Farooq, MD2, Ashish Dhawan, MBBS3, Ammad Javaid. Chaudhary, MD4, Laraib Fatima. Sheikh, 5, Nosheen Hafeez, MD6, Tilak Upendra. Shah, MD7
1Rochester General Hospital, Rochester, NY; 2SSM Health Saint Louis University Hospital, St. Louis, MO; 3Gian Sagar Medical College and Hospital, Chandigarh, Chandigarh, India; 4Henry Ford Health, Detroit, MI; 5Lahore Medical and Dental College, Rochester, NY; 6Baptist Health-University of Arkansas for Medical Sciences, North Little Rock, AR; 7Cleveland Clinic Florida, Weston, FL
Introduction: Acute cholangitis (AC) is a lethal infection of the biliary tract with varying degrees of severity. While endoscopic retrograde cholangiopancreatography (ERCP) remains the mainstay drainage modality, the timing of drainage is contingent on the severity of AC. Though frailty is linked to poor outcomes in general, its implications for AC patients remain unexplored. This study aims to bridge this research gap by conducting a nationwide analysis.
Methods: Using the National Inpatient Sample Database (NIS) from 2017 to 2020, we employed the International Classification of Diseases, 10th revision, Clinical Modifications (ICD-10-CM) codes to identify adult patients (age >18 years) admitted with AC. We further stratified AC hospitalizations based on the presence of frailty. Utilizing a multivariate regression model, we compared the impact of frailty on the outcomes and procedural performance of AC patients. STATA 14.2 was utilized for statistical analysis.
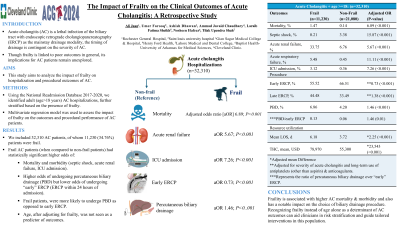
Results: We included 32,310 AC patients, out of whom 11,230 (34.76%) patients were frail. After adjusting for confounding variables, in-hospital mortality of AC was significantly higher in frail patients (adjusted odds ratio [aOR] 3.95; P< 0.01) (Table 1). Additionally, frail patients were found to have significantly higher odds of septic shock (aOR 16.26, P< 0.01), acute renal failure (aOR 5.71, P< 0.01), acute respiratory failure (aOR 10.51, P< 0.01), vasopressor requirement (aOR 5.02, P< 0.01), and mechanical ventilation (aOR 11.61, P< 0.01). From a procedural viewpoint, frail patients had higher odds of undergoing percutaneous biliary drainage (PBD) but lower odds of undergoing “early” ERCP (ERCP within 24 hours of admission). We also found that frail patients, when compared to their non-frail counterparts, were more likely to undergo PBD as opposed to early ERCP (aOR 1.46, P= 0.01). Age, after adjusting for frailty, was not seen as a predictor of outcomes. Finally, resource utilization was also significantly higher among frail patients.
Discussion: Frailty independently predicts poor AC outcomes and has a notable impact on the choice of biliary drainage procedure. Recognizing frailty instead of age alone as a determinant of AC outcomes can aid clinicians in risk stratification and guide tailored interventions in this population.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ali Jaan, MD1, Umer Farooq, MD2, Ashish Dhawan, MBBS3, Ammad Javaid. Chaudhary, MD4, Laraib Fatima. Sheikh, 5, Nosheen Hafeez, MD6, Tilak Upendra. Shah, MD7. P0044 - The Impact of Frailty on the Clinical Outcomes of Acute Cholangitis: A Retrospective Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Rochester General Hospital, Rochester, NY; 2SSM Health Saint Louis University Hospital, St. Louis, MO; 3Gian Sagar Medical College and Hospital, Chandigarh, Chandigarh, India; 4Henry Ford Health, Detroit, MI; 5Lahore Medical and Dental College, Rochester, NY; 6Baptist Health-University of Arkansas for Medical Sciences, North Little Rock, AR; 7Cleveland Clinic Florida, Weston, FL
Introduction: Acute cholangitis (AC) is a lethal infection of the biliary tract with varying degrees of severity. While endoscopic retrograde cholangiopancreatography (ERCP) remains the mainstay drainage modality, the timing of drainage is contingent on the severity of AC. Though frailty is linked to poor outcomes in general, its implications for AC patients remain unexplored. This study aims to bridge this research gap by conducting a nationwide analysis.
Methods: Using the National Inpatient Sample Database (NIS) from 2017 to 2020, we employed the International Classification of Diseases, 10th revision, Clinical Modifications (ICD-10-CM) codes to identify adult patients (age >18 years) admitted with AC. We further stratified AC hospitalizations based on the presence of frailty. Utilizing a multivariate regression model, we compared the impact of frailty on the outcomes and procedural performance of AC patients. STATA 14.2 was utilized for statistical analysis.
Results: We included 32,310 AC patients, out of whom 11,230 (34.76%) patients were frail. After adjusting for confounding variables, in-hospital mortality of AC was significantly higher in frail patients (adjusted odds ratio [aOR] 3.95; P< 0.01) (Table 1). Additionally, frail patients were found to have significantly higher odds of septic shock (aOR 16.26, P< 0.01), acute renal failure (aOR 5.71, P< 0.01), acute respiratory failure (aOR 10.51, P< 0.01), vasopressor requirement (aOR 5.02, P< 0.01), and mechanical ventilation (aOR 11.61, P< 0.01). From a procedural viewpoint, frail patients had higher odds of undergoing percutaneous biliary drainage (PBD) but lower odds of undergoing “early” ERCP (ERCP within 24 hours of admission). We also found that frail patients, when compared to their non-frail counterparts, were more likely to undergo PBD as opposed to early ERCP (aOR 1.46, P= 0.01). Age, after adjusting for frailty, was not seen as a predictor of outcomes. Finally, resource utilization was also significantly higher among frail patients.
Discussion: Frailty independently predicts poor AC outcomes and has a notable impact on the choice of biliary drainage procedure. Recognizing frailty instead of age alone as a determinant of AC outcomes can aid clinicians in risk stratification and guide tailored interventions in this population.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ali Jaan indicated no relevant financial relationships.
Umer Farooq indicated no relevant financial relationships.
Ashish Dhawan indicated no relevant financial relationships.
Ammad Chaudhary indicated no relevant financial relationships.
Laraib Sheikh indicated no relevant financial relationships.
Nosheen Hafeez indicated no relevant financial relationships.
Tilak Shah indicated no relevant financial relationships.
Ali Jaan, MD1, Umer Farooq, MD2, Ashish Dhawan, MBBS3, Ammad Javaid. Chaudhary, MD4, Laraib Fatima. Sheikh, 5, Nosheen Hafeez, MD6, Tilak Upendra. Shah, MD7. P0044 - The Impact of Frailty on the Clinical Outcomes of Acute Cholangitis: A Retrospective Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
