Sunday Poster Session
Category: Biliary/Pancreas
P0067 - To Consult, or to Not Consult? That is the Question
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Naomi Reddy-Patel, MD
St. Luke's University Hospital
Bethlehem, PA
Presenting Author(s)
Naomi Reddy-Patel, MD1, Janak Bahirwani, MD2, Nishit Patel, MD2, Frank Lin, DO3, Het Patel, DO1, Kimberly Chaput, DO2
1St. Luke's University Hospital, Bethlehem, PA; 2St. Luke's University Health Network, Bethlehem, PA; 3St. Luke's University Health Network, Allentown, PA
Introduction: Despite a increase in reported cases and enhanced access to care, acute pancreatitis remains associated with significant morbidity and mortality. Notably, recent audits reveal substantial noncompliance with evidence-based recommendations in clinical management, emphasizing the need for clear and practical guidelines. This study addresses a crucial gap by investigating the GI consultation practices for acute pancreatitis, aiming to contribute valuable insights to enhance adherence to evidence-based recommendations in the diagnosis and management of this condition
Methods: This is a retrospective chart review looking at 150 patients diagnosed with acute pancreatitis at one institution over Jan 2023 to June 2023. Variables were obtained including whether GI was consulted upon admission. Complications such as ICU admission, development of hemorrhagic pancreatitis, acute kidney injury, or death were all obtained. Two tailed Z test was performed on the data
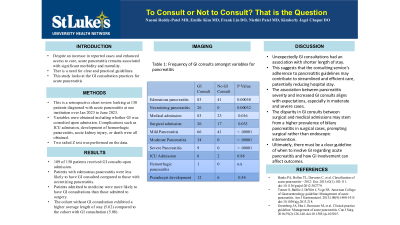
Results: In the study, 109 of 150 patients received GI consults upon admission. Table 1 revealed a statistically significant difference between type of pancreatitis and GI consults. Patients with edematous pancreatitis were less likely to have GI consulted compared to those with necrotizing pancreatitis. Notably, patients admitted to medicine were more likely to have GI consultations than those admitted to surgery. The frequency of GI consultations correlated with the severity of pancreatitis. Additionally, the cohort without GI consultation exhibited a higher average length of stay (5.62) compared to the cohort with GI consultation (5.08)
Discussion: The unexpected shorter length of stay for the group with GI consults challenges the assumption that more severe pancreatitis cases requiring GI intervention would lead to prolonged hospitalization. This counterintuitive outcome suggests that the consulting service's adherence to pancreatitis guidelines may contribute to streamlined and efficient care, potentially reducing hospital stay. The association between pancreatitis severity and increased GI consults aligns with expectations, especially in moderate and severe cases. The intriguing disparity in GI consults between surgical and medical admissions may stem from a higher prevalence of biliary pancreatitis in surgical cases, prompting surgical rather than endoscopic intervention. Ultimately, there must be a clear guideline of when to involve GI regarding acute pancreatitis and how GI involvement can affect outcomes
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Naomi Reddy-Patel, MD1, Janak Bahirwani, MD2, Nishit Patel, MD2, Frank Lin, DO3, Het Patel, DO1, Kimberly Chaput, DO2. P0067 - To Consult, or to Not Consult? That is the Question, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1St. Luke's University Hospital, Bethlehem, PA; 2St. Luke's University Health Network, Bethlehem, PA; 3St. Luke's University Health Network, Allentown, PA
Introduction: Despite a increase in reported cases and enhanced access to care, acute pancreatitis remains associated with significant morbidity and mortality. Notably, recent audits reveal substantial noncompliance with evidence-based recommendations in clinical management, emphasizing the need for clear and practical guidelines. This study addresses a crucial gap by investigating the GI consultation practices for acute pancreatitis, aiming to contribute valuable insights to enhance adherence to evidence-based recommendations in the diagnosis and management of this condition
Methods: This is a retrospective chart review looking at 150 patients diagnosed with acute pancreatitis at one institution over Jan 2023 to June 2023. Variables were obtained including whether GI was consulted upon admission. Complications such as ICU admission, development of hemorrhagic pancreatitis, acute kidney injury, or death were all obtained. Two tailed Z test was performed on the data
Results: In the study, 109 of 150 patients received GI consults upon admission. Table 1 revealed a statistically significant difference between type of pancreatitis and GI consults. Patients with edematous pancreatitis were less likely to have GI consulted compared to those with necrotizing pancreatitis. Notably, patients admitted to medicine were more likely to have GI consultations than those admitted to surgery. The frequency of GI consultations correlated with the severity of pancreatitis. Additionally, the cohort without GI consultation exhibited a higher average length of stay (5.62) compared to the cohort with GI consultation (5.08)
Discussion: The unexpected shorter length of stay for the group with GI consults challenges the assumption that more severe pancreatitis cases requiring GI intervention would lead to prolonged hospitalization. This counterintuitive outcome suggests that the consulting service's adherence to pancreatitis guidelines may contribute to streamlined and efficient care, potentially reducing hospital stay. The association between pancreatitis severity and increased GI consults aligns with expectations, especially in moderate and severe cases. The intriguing disparity in GI consults between surgical and medical admissions may stem from a higher prevalence of biliary pancreatitis in surgical cases, prompting surgical rather than endoscopic intervention. Ultimately, there must be a clear guideline of when to involve GI regarding acute pancreatitis and how GI involvement can affect outcomes
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Naomi Reddy-Patel indicated no relevant financial relationships.
Janak Bahirwani indicated no relevant financial relationships.
Nishit Patel indicated no relevant financial relationships.
Frank Lin indicated no relevant financial relationships.
Het Patel indicated no relevant financial relationships.
Kimberly Chaput indicated no relevant financial relationships.
Naomi Reddy-Patel, MD1, Janak Bahirwani, MD2, Nishit Patel, MD2, Frank Lin, DO3, Het Patel, DO1, Kimberly Chaput, DO2. P0067 - To Consult, or to Not Consult? That is the Question, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
