Sunday Poster Session
Category: Biliary/Pancreas
P0096 - PEG Tube-Associated Obstructive Pancreatitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- RO
Riley Ostdiek, MD
University of South Florida
Tampa, FL
Presenting Author(s)
Sonya Bhaskar, MD1, Riley Ostdiek, MD1, Brijesh Patel, MD2
1University of South Florida, Tampa, FL; 2University of South Florida, James A. Haley VA Hospital, Tampa, FL
Introduction: Percutaneous endoscopic gastrostomy (PEG) tubes are commonly used for long-term enteral nutrition in many clinical settings. In the US, over 160,000 PEG tubes are placed annually, and the majority of PEG tubes are placed by gastroenterologists. Common complications of PEG tubes include abdominal wall pain, gastric content leakage, bleeding, and infection. In this case report, we review a unique and rare complication: migration of PEG tube causing obstructive pancreatitis.
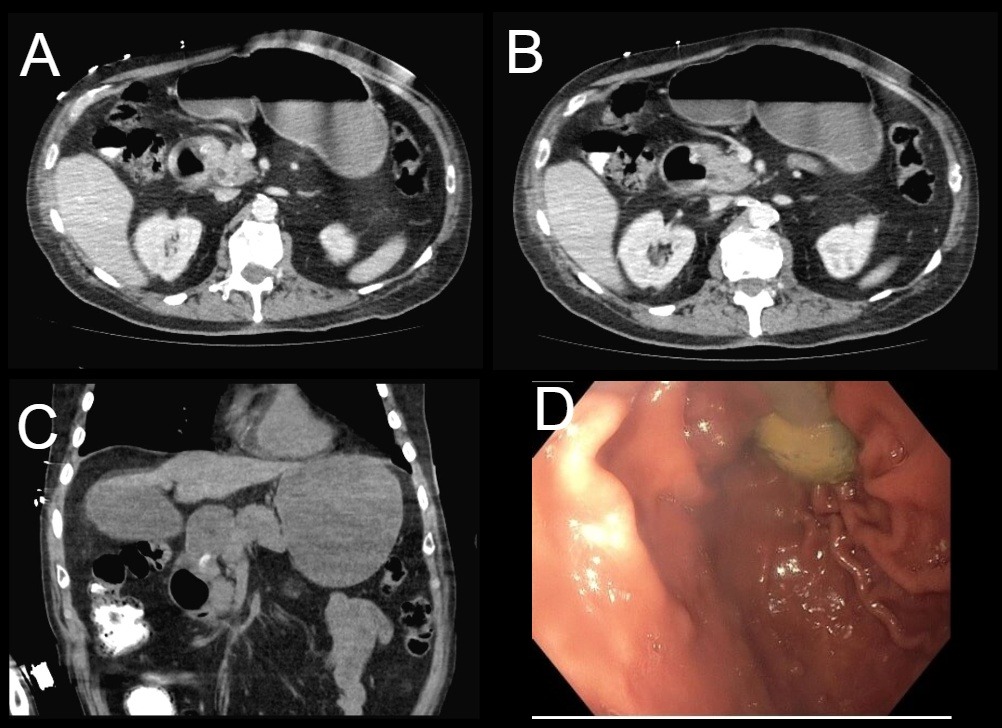
Case Description/Methods: A 69-year-old male with a past medical history of traumatic brain injury complicated by cognitive impairment and oropharyngeal dysphagia presented to the emergency department due to tachycardia, vomiting, and PEG tube leakage. The PEG tube was originally placed 3 cm from the abdominal wall, whereas on this presentation the PEG tube was noted to be 6 cm from the abdominal wall. Initial labs demonstrated leukocytosis of 15.67 x109/L, lipase of >3000 U/L, hypercalcemia of 10.4 mg/dL, and mild hyperbilirubinemia of 1.4 mg/dL. CT pancreas demonstrated G-tube bulb migration causing mechanical obstruction at the pancreatico-biliary junction resulting in dilated common bile and pancreatic ducts and causing gastric outlet obstruction.
Esophagogastroduodenoscopy was completed on day of admission which demonstrated the G-tube in the body of the stomach with the inflated balloon near the pylorus. G-tube was snared and removed. Replacement PEG tube was inserted and fixed to 4 cm at conclusion of procedure.
Following removal of G-tube, lab values including lipase and white blood cell count rapidly down trended. The patient became more interactive and near-baseline. Replacement PEG tube remained patent and patient tolerated resumption of enteral feeding.
Discussion: Percutaneous endoscopic gastrostomy tube placement is a common method for enteral nutritional support and is generally safe and well-tolerated. PEG tube migration is an uncommon complication, and PEG tube migration causing common bile duct obstruction and pancreatitis is extremely rare. Fewer than 20 cases of G-tube associated obstructive pancreatitis have been reported.
Many prior cases were related to use of non-bumpered tubes including foley catheters, with a small subset of cases presenting like this one.
This case highlights a rare complication of a common procedure and highlights the importance of utilizing imaging, laboratory studies, and interprofessional communication to promptly address life-threatening conditions.
Disclosures:
Sonya Bhaskar, MD1, Riley Ostdiek, MD1, Brijesh Patel, MD2. P0096 - PEG Tube-Associated Obstructive Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of South Florida, Tampa, FL; 2University of South Florida, James A. Haley VA Hospital, Tampa, FL
Introduction: Percutaneous endoscopic gastrostomy (PEG) tubes are commonly used for long-term enteral nutrition in many clinical settings. In the US, over 160,000 PEG tubes are placed annually, and the majority of PEG tubes are placed by gastroenterologists. Common complications of PEG tubes include abdominal wall pain, gastric content leakage, bleeding, and infection. In this case report, we review a unique and rare complication: migration of PEG tube causing obstructive pancreatitis.
Case Description/Methods: A 69-year-old male with a past medical history of traumatic brain injury complicated by cognitive impairment and oropharyngeal dysphagia presented to the emergency department due to tachycardia, vomiting, and PEG tube leakage. The PEG tube was originally placed 3 cm from the abdominal wall, whereas on this presentation the PEG tube was noted to be 6 cm from the abdominal wall. Initial labs demonstrated leukocytosis of 15.67 x109/L, lipase of >3000 U/L, hypercalcemia of 10.4 mg/dL, and mild hyperbilirubinemia of 1.4 mg/dL. CT pancreas demonstrated G-tube bulb migration causing mechanical obstruction at the pancreatico-biliary junction resulting in dilated common bile and pancreatic ducts and causing gastric outlet obstruction.
Esophagogastroduodenoscopy was completed on day of admission which demonstrated the G-tube in the body of the stomach with the inflated balloon near the pylorus. G-tube was snared and removed. Replacement PEG tube was inserted and fixed to 4 cm at conclusion of procedure.
Following removal of G-tube, lab values including lipase and white blood cell count rapidly down trended. The patient became more interactive and near-baseline. Replacement PEG tube remained patent and patient tolerated resumption of enteral feeding.
Discussion: Percutaneous endoscopic gastrostomy tube placement is a common method for enteral nutritional support and is generally safe and well-tolerated. PEG tube migration is an uncommon complication, and PEG tube migration causing common bile duct obstruction and pancreatitis is extremely rare. Fewer than 20 cases of G-tube associated obstructive pancreatitis have been reported.
Many prior cases were related to use of non-bumpered tubes including foley catheters, with a small subset of cases presenting like this one.
This case highlights a rare complication of a common procedure and highlights the importance of utilizing imaging, laboratory studies, and interprofessional communication to promptly address life-threatening conditions.
Figure: Images A, B, C: Transverse and coronal views of PEG tube with extension into small bowel.
Image D: Endoscopic view of PEG tube prior to removal.
Image D: Endoscopic view of PEG tube prior to removal.
Disclosures:
Sonya Bhaskar indicated no relevant financial relationships.
Riley Ostdiek indicated no relevant financial relationships.
Brijesh Patel indicated no relevant financial relationships.
Sonya Bhaskar, MD1, Riley Ostdiek, MD1, Brijesh Patel, MD2. P0096 - PEG Tube-Associated Obstructive Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

