Sunday Poster Session
Category: Biliary/Pancreas
P0123 - A Rare Case of Biliary Cast Syndrome
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Rishika Trivedi, MD
DHR Health
Edinburg, TX
Presenting Author(s)
Rishika Trivedi, MD1, Mahmoud Barbarawi, MD2, Asif Zamir, MD, FACG3
1DHR Health, Edinburg, TX; 2DHR Health Gastroenterology, McAllen, TX; 3DHR Health Gastroenterology, Edinburg, TX
Introduction: Biliary cast syndrome (BCS) is a rare condition characterized by the formation of casts within the biliary ducts, leading to obstruction and potential biliary complications. BCS is predominantly observed in liver transplant recipients, with an incidence of up to 5–18%. The incidence remains poorly defined in non-transplant patients, making our case a rare presentation.
Case Description/Methods: A 48-year-old male with a past medical history of diabetes, hypertension and cirrhosis underwent open cholecystectomy after presenting with symptoms suggestive of acute cholecystitis. The post-op course was complicated with bile leak and unresolving jaundice despite ERCP and biliary stenting in another institution. The patient was then transferred to our institution for a higher level of care.
At the time of admission, the lab workup showed a WBC of 13.1K, AST 135, ALT 89, ALP 1680 and total bilirubin of 19.3. CT abdomen and pelvis showed stents in place but persistent bilobar intrahepatic biliary ductal dilatation (Fig. 1). ERCP was performed (Fig. 2) with removal of previously placed stents, and the cholangiogram revealed multiple filling defects in both the right and left hepatic ducts. Spyglass cholangioscopy showed impacted stones in the right and left systems. Electrohydraulic Lithotripsy was performed, which led to the fragmentation of several stones. However, as we advanced further up with the spyglass scope, the whole biliary system appeared to be impacted with stones (Fig. 3A). At this point, 2 biliary plastic stents of sizes 10 Fr x 15 cm and 8.5 Fr x 15 cm were placed in the right and left hepatic ducts, respectively (Fig. 3B). There were no postoperative complications, and a decision was made to consult the hepatobiliary service. The patient underwent intrahepatic hepaticojejunostomy, bile duct exploration, and removal of biliary casts from the intrahepatic bile ducts (Fig. 4). Postoperatively, the liver chemistries significantly improved. Bile duct pathology showed acute and chronic inflammation with granulomas (Fig. 5).
Discussion: We present a unique case of BCS in a non-transplant patient requiring a multidisciplinary collaboration. Our aim is to outline a comprehensive approach for this condition, thus adding valuable insights to the existing sparse literature.

Disclosures:
Rishika Trivedi, MD1, Mahmoud Barbarawi, MD2, Asif Zamir, MD, FACG3. P0123 - A Rare Case of Biliary Cast Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1DHR Health, Edinburg, TX; 2DHR Health Gastroenterology, McAllen, TX; 3DHR Health Gastroenterology, Edinburg, TX
Introduction: Biliary cast syndrome (BCS) is a rare condition characterized by the formation of casts within the biliary ducts, leading to obstruction and potential biliary complications. BCS is predominantly observed in liver transplant recipients, with an incidence of up to 5–18%. The incidence remains poorly defined in non-transplant patients, making our case a rare presentation.
Case Description/Methods: A 48-year-old male with a past medical history of diabetes, hypertension and cirrhosis underwent open cholecystectomy after presenting with symptoms suggestive of acute cholecystitis. The post-op course was complicated with bile leak and unresolving jaundice despite ERCP and biliary stenting in another institution. The patient was then transferred to our institution for a higher level of care.
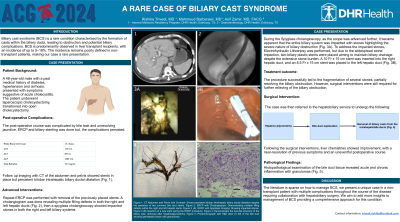
At the time of admission, the lab workup showed a WBC of 13.1K, AST 135, ALT 89, ALP 1680 and total bilirubin of 19.3. CT abdomen and pelvis showed stents in place but persistent bilobar intrahepatic biliary ductal dilatation (Fig. 1). ERCP was performed (Fig. 2) with removal of previously placed stents, and the cholangiogram revealed multiple filling defects in both the right and left hepatic ducts. Spyglass cholangioscopy showed impacted stones in the right and left systems. Electrohydraulic Lithotripsy was performed, which led to the fragmentation of several stones. However, as we advanced further up with the spyglass scope, the whole biliary system appeared to be impacted with stones (Fig. 3A). At this point, 2 biliary plastic stents of sizes 10 Fr x 15 cm and 8.5 Fr x 15 cm were placed in the right and left hepatic ducts, respectively (Fig. 3B). There were no postoperative complications, and a decision was made to consult the hepatobiliary service. The patient underwent intrahepatic hepaticojejunostomy, bile duct exploration, and removal of biliary casts from the intrahepatic bile ducts (Fig. 4). Postoperatively, the liver chemistries significantly improved. Bile duct pathology showed acute and chronic inflammation with granulomas (Fig. 5).
Discussion: We present a unique case of BCS in a non-transplant patient requiring a multidisciplinary collaboration. Our aim is to outline a comprehensive approach for this condition, thus adding valuable insights to the existing sparse literature.

Figure: Figure 1: CT Abdomen and Pelvis with Contrast- Shows persistent bilobar intrahepatic biliary ductal dilatation despite the presence of two common bile duct stents. Figure 2: ERCP with Cholangiogram: Demonstrating multiple filling defects within the right and left hepatic ducts. Figure 3 (A): ERCP with SpyGlass Imaging: Showing impacted stones. Figure 3 (B) Insertion of a new stent during the ERCP procedure. Figure 4: Biliary Cast - Demonstrates the tree-like structure of the biliary cast, removed after hepaticojejunostomy. Figure 5: Photomicrograph with H&E stain (X 20) of the bile duct showing perihepatic tissue with granulomas.
Disclosures:
Rishika Trivedi indicated no relevant financial relationships.
Mahmoud Barbarawi indicated no relevant financial relationships.
Asif Zamir indicated no relevant financial relationships.
Rishika Trivedi, MD1, Mahmoud Barbarawi, MD2, Asif Zamir, MD, FACG3. P0123 - A Rare Case of Biliary Cast Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

