Sunday Poster Session
Category: Biliary/Pancreas
P0126 - Unveiling the Uncommon: A Rare Case of Infected Intraductal Papillary Mucinous Neoplasm of Pancreas
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Taha Bin Arif, MBBS, MD
Sinai Hospital
Baltimore, MD
Presenting Author(s)
Taha Bin Arif, MBBS, MD1, Rida Ihsan, MBBS, MD1, Asad Ur Rahman, MD2, Muhammad Zarrar Khan, MD3
1Sinai Hospital, Baltimore, MD; 2Cleveland Clinic Florida, Weston, FL; 3Henry Ford Hospital, Royal Oak, MI
Introduction: Intraductal papillary mucinous neoplasm (IPMN) of the pancreas involves papillary growths within its ductal system. Complications, though extremely rare, include infections due to rupture, fistulization, or malignant transformation. We report a case of infected IPMN in a 76-year-old male with recurrent abdominal pain, treated successfully with cyst drainage and antibiotics.
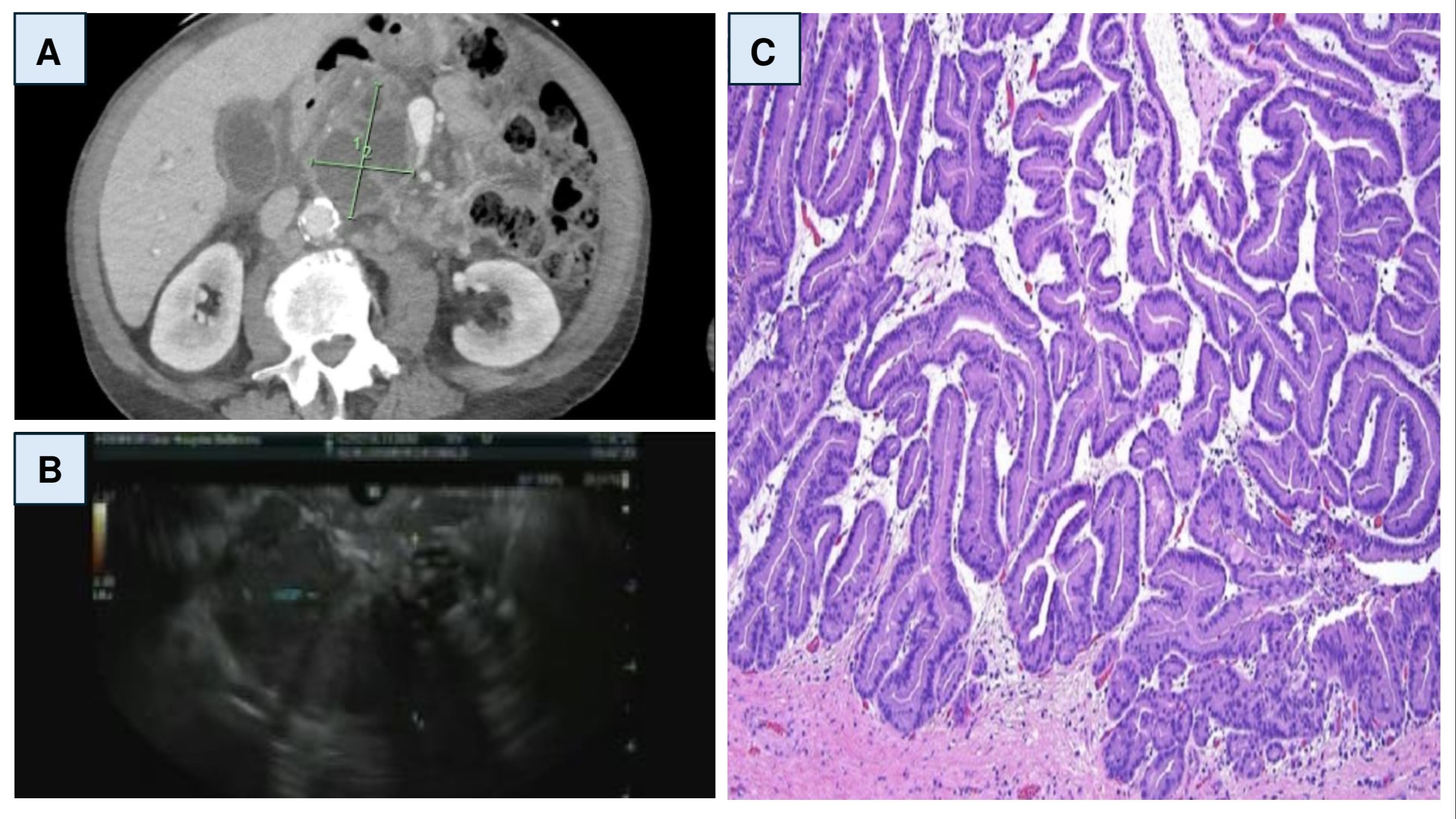
Case Description/Methods: A 76-year-old male with a history of COPD, prediabetes, and pancreatic cyst (on pancrelipase) presented with diffuse abdominal pain for 3 hours. He had a previous presentation 5 days ago with worsening abdominal pain, fever, chills, and nausea. Magnetic Resonance Cholangiopancreatography (MRCP) at that time showed a cystic mass affecting the left renal vein and pancreas, prompting a referral for endoscopic ultrasound (EUS). On examination, he had minor wheezes and mild diffuse abdominal tenderness. Labs showed elevated liver biochemistry panel, leukocytosis, and anemia. CT scan revealed a possible abscess connected to the known pancreatic cyst. Abdominal ultrasound suggested acute cholecystitis possibly related to the pancreatic mass. EUS showed pancreatic duct dilation and a heterogeneous lesion posterior to the left lobe of the liver. Fine needle aspiration (FNA) revealed inflammatory debris and pseudomonas aeruginosa growth in the drainage culture. Pancreatic cyst CEA was elevated with low amylase, indicating an infected IPMN. Antibiotics were continued, and the patient was discharged with oral therapy (ciprofloxacin and metronidazole) for follow-up imaging with gastroenterology.
Discussion: This is the fourth known case of spontaneous IPMN infection. Previous cases involved patients with sepsis and multilocular cystic tumors, with one case being asymptomatic. All cases were treated with cyst drainage and antibiotics. Our case showed infection with pseudomonas aeruginosa. The pathogenesis is unclear, potentially involving retrograde bacterial translocation due to papillary orifice dilation or other factors like alcohol-induced pancreatitis or immunosuppression associated with diabetes. Imaging may show unusual fluid layering, with EUS revealing clumped mucin. Management typically involves drainage and antibiotics, with considerations for resection in cases of dysplastic transformation. Our case did not require resection as no malignancy was observed. Spontaneous IPMN infection is rare, varying from asymptomatic to severe sepsis. EUS-guided FNA can aid in diagnosis and management.
Disclosures:
Taha Bin Arif, MBBS, MD1, Rida Ihsan, MBBS, MD1, Asad Ur Rahman, MD2, Muhammad Zarrar Khan, MD3. P0126 - Unveiling the Uncommon: A Rare Case of Infected Intraductal Papillary Mucinous Neoplasm of Pancreas, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Sinai Hospital, Baltimore, MD; 2Cleveland Clinic Florida, Weston, FL; 3Henry Ford Hospital, Royal Oak, MI
Introduction: Intraductal papillary mucinous neoplasm (IPMN) of the pancreas involves papillary growths within its ductal system. Complications, though extremely rare, include infections due to rupture, fistulization, or malignant transformation. We report a case of infected IPMN in a 76-year-old male with recurrent abdominal pain, treated successfully with cyst drainage and antibiotics.
Case Description/Methods: A 76-year-old male with a history of COPD, prediabetes, and pancreatic cyst (on pancrelipase) presented with diffuse abdominal pain for 3 hours. He had a previous presentation 5 days ago with worsening abdominal pain, fever, chills, and nausea. Magnetic Resonance Cholangiopancreatography (MRCP) at that time showed a cystic mass affecting the left renal vein and pancreas, prompting a referral for endoscopic ultrasound (EUS). On examination, he had minor wheezes and mild diffuse abdominal tenderness. Labs showed elevated liver biochemistry panel, leukocytosis, and anemia. CT scan revealed a possible abscess connected to the known pancreatic cyst. Abdominal ultrasound suggested acute cholecystitis possibly related to the pancreatic mass. EUS showed pancreatic duct dilation and a heterogeneous lesion posterior to the left lobe of the liver. Fine needle aspiration (FNA) revealed inflammatory debris and pseudomonas aeruginosa growth in the drainage culture. Pancreatic cyst CEA was elevated with low amylase, indicating an infected IPMN. Antibiotics were continued, and the patient was discharged with oral therapy (ciprofloxacin and metronidazole) for follow-up imaging with gastroenterology.
Discussion: This is the fourth known case of spontaneous IPMN infection. Previous cases involved patients with sepsis and multilocular cystic tumors, with one case being asymptomatic. All cases were treated with cyst drainage and antibiotics. Our case showed infection with pseudomonas aeruginosa. The pathogenesis is unclear, potentially involving retrograde bacterial translocation due to papillary orifice dilation or other factors like alcohol-induced pancreatitis or immunosuppression associated with diabetes. Imaging may show unusual fluid layering, with EUS revealing clumped mucin. Management typically involves drainage and antibiotics, with considerations for resection in cases of dysplastic transformation. Our case did not require resection as no malignancy was observed. Spontaneous IPMN infection is rare, varying from asymptomatic to severe sepsis. EUS-guided FNA can aid in diagnosis and management.
Figure: Figure 1A: CT abdomen showing 6 cm thick-walled septated cystic mass in the region of inferior pancreatic head and uncinate process, indicative of intraductal papillary mucinous neoplasm. 1B: Endoscopic ultrasound showing cystic necrotic appearing lesion in pancreatic head and uncinate process of pancreas. 1C: Histopathological specimen of intraductal papillary mucinous neoplasm of pancreas.
Disclosures:
Taha Bin Arif indicated no relevant financial relationships.
Rida Ihsan indicated no relevant financial relationships.
Asad Ur Rahman: Abbvie – Speakers Bureau.
Muhammad Zarrar Khan indicated no relevant financial relationships.
Taha Bin Arif, MBBS, MD1, Rida Ihsan, MBBS, MD1, Asad Ur Rahman, MD2, Muhammad Zarrar Khan, MD3. P0126 - Unveiling the Uncommon: A Rare Case of Infected Intraductal Papillary Mucinous Neoplasm of Pancreas, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
