Sunday Poster Session
Category: Biliary/Pancreas
P0130 - Splenic Vascular Laceration After Endoscopic Necrosectomy and Cyst-Gastrostomy Placement
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Hayden E. Rotramel, MD
SSM Health St. Louis University Hospital
St. Louis, MO
Presenting Author(s)
Hayden Rotramel, MD1, Ryan Plunkett, MD2, Ameya Deshmukh, DO2, Michelle Baliss, DO3, Zarir Ahmed, DO3, Antonio Cheesman, MD3
1SSM Health St. Louis University Hospital, St. Louis, MO; 2Saint Louis University School of Medicine, St. Louis, MO; 3SSM Health Saint Louis University Hospital, St. Louis, MO
Introduction: Walled-off pancreatic necrosis (WOPN) is a rare complication of acute or chronic pancreatitis. Previously, treatment most commonly involved surgical intervention, however, it can now be treated with endoscopic pancreatic necrosectomy and cyst-gastrostomy. Although these approaches appear to possess a more desirable safety profile, they do still carry the risk of severe complications. Here, we present a complication of these procedures.
Case Description/Methods: A 45-year-old man with a history of chronic pancreatitis presented with acute-onset hematemesis, melena, and abdominal pain. 2 weeks prior, the patient had undergone magnetic resonance cholangiopancreatography which showed a 6.7 x 3.4 cm collection of material within the pancreatic tail. Endoscopic ultrasound (EUS) with fine needle aspiration revealed necrotic debris. Due to ongoing pain the patient underwent EUS-guided cyst-gastrostomy (CG) and endoscopic pancreatic necrosectomy (EPN). The patient tolerated these interventions well and was discharged home with outpatient follow up. On presentation to our institution, the patient met criteria for sepsis, raising concern for a complication related to the previous procedures. Computerized tomography angiography (CTA) of the abdomen and pelvis showed that the pigtail stent had migrated into the splenic arterial branches at the splenic hilum, resulting in splenic artery injury and large splenic infarct. There was also abundant mixed hyperdense material within the stomach suggestive of hemorrhagic contents, likely representing splenic hilum vascular injury that may have decompressed into the stomach. Interventional radiology was consulted and emergently performed coil embolization of the splenic artery. Following the procedure the patient’s symptoms resolved and he remained hemodynamically stable.
Discussion: EPN and CG are highly effective in the treatment of WOPN and have also been shown to have fewer rates of complications when compared to surgical interventions. However, this case highlights the need for awareness of possible dangerous complications necessitating early intervention. Splenic vascular injury and infarcts, can occur as immediate and delayed complications, thus, endoscopists should be vigilant of their occurrence post-procedure. Lastly, it may be beneficial to standardize these procedures on a wider scale to reduce the rates of these complications.

Disclosures:
Hayden Rotramel, MD1, Ryan Plunkett, MD2, Ameya Deshmukh, DO2, Michelle Baliss, DO3, Zarir Ahmed, DO3, Antonio Cheesman, MD3. P0130 - Splenic Vascular Laceration After Endoscopic Necrosectomy and Cyst-Gastrostomy Placement, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1SSM Health St. Louis University Hospital, St. Louis, MO; 2Saint Louis University School of Medicine, St. Louis, MO; 3SSM Health Saint Louis University Hospital, St. Louis, MO
Introduction: Walled-off pancreatic necrosis (WOPN) is a rare complication of acute or chronic pancreatitis. Previously, treatment most commonly involved surgical intervention, however, it can now be treated with endoscopic pancreatic necrosectomy and cyst-gastrostomy. Although these approaches appear to possess a more desirable safety profile, they do still carry the risk of severe complications. Here, we present a complication of these procedures.
Case Description/Methods: A 45-year-old man with a history of chronic pancreatitis presented with acute-onset hematemesis, melena, and abdominal pain. 2 weeks prior, the patient had undergone magnetic resonance cholangiopancreatography which showed a 6.7 x 3.4 cm collection of material within the pancreatic tail. Endoscopic ultrasound (EUS) with fine needle aspiration revealed necrotic debris. Due to ongoing pain the patient underwent EUS-guided cyst-gastrostomy (CG) and endoscopic pancreatic necrosectomy (EPN). The patient tolerated these interventions well and was discharged home with outpatient follow up. On presentation to our institution, the patient met criteria for sepsis, raising concern for a complication related to the previous procedures. Computerized tomography angiography (CTA) of the abdomen and pelvis showed that the pigtail stent had migrated into the splenic arterial branches at the splenic hilum, resulting in splenic artery injury and large splenic infarct. There was also abundant mixed hyperdense material within the stomach suggestive of hemorrhagic contents, likely representing splenic hilum vascular injury that may have decompressed into the stomach. Interventional radiology was consulted and emergently performed coil embolization of the splenic artery. Following the procedure the patient’s symptoms resolved and he remained hemodynamically stable.
Discussion: EPN and CG are highly effective in the treatment of WOPN and have also been shown to have fewer rates of complications when compared to surgical interventions. However, this case highlights the need for awareness of possible dangerous complications necessitating early intervention. Splenic vascular injury and infarcts, can occur as immediate and delayed complications, thus, endoscopists should be vigilant of their occurrence post-procedure. Lastly, it may be beneficial to standardize these procedures on a wider scale to reduce the rates of these complications.

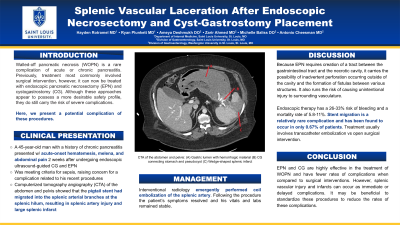
Figure: (A) Gastric lumen with hemorrhagic material (B) Cyst-gastrostomy connecting stomach and pseudocyst (C) Wedge-shaped splenic infarct
Disclosures:
Hayden Rotramel indicated no relevant financial relationships.
Ryan Plunkett indicated no relevant financial relationships.
Ameya Deshmukh indicated no relevant financial relationships.
Michelle Baliss indicated no relevant financial relationships.
Zarir Ahmed indicated no relevant financial relationships.
Antonio Cheesman indicated no relevant financial relationships.
Hayden Rotramel, MD1, Ryan Plunkett, MD2, Ameya Deshmukh, DO2, Michelle Baliss, DO3, Zarir Ahmed, DO3, Antonio Cheesman, MD3. P0130 - Splenic Vascular Laceration After Endoscopic Necrosectomy and Cyst-Gastrostomy Placement, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
