Sunday Poster Session
Category: Biliary/Pancreas
P0131 - A Rare Complication of Chronic Pancreatitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Hayden E. Rotramel, MD
SSM Health St. Louis University Hospital
St. Louis, MO
Presenting Author(s)
Hayden Rotramel, MD1, Ryan Plunkett, MD2, Ameya Deshmukh, DO2, Mahmoud Y. Madi, MD3, Wissam Kiwan, MD4
1SSM Health St. Louis University Hospital, St. Louis, MO; 2Saint Louis University School of Medicine, St. Louis, MO; 3SSM Health Saint Louis University Hospital, St. Louis, MO; 4Saint Louis University, St. Louis, MO
Introduction: The formation of pancreaticopleural fistulas (PPFs) is an extremely rare complication of chronic pancreatitis. It can be difficult to diagnose this condition as patients often do not present with the typical signs or symptoms associated with pancreatitis. Here, we present a case of a woman presenting with pulmonary symptoms who was later found to have PPF secondary to chronic pancreatitis.
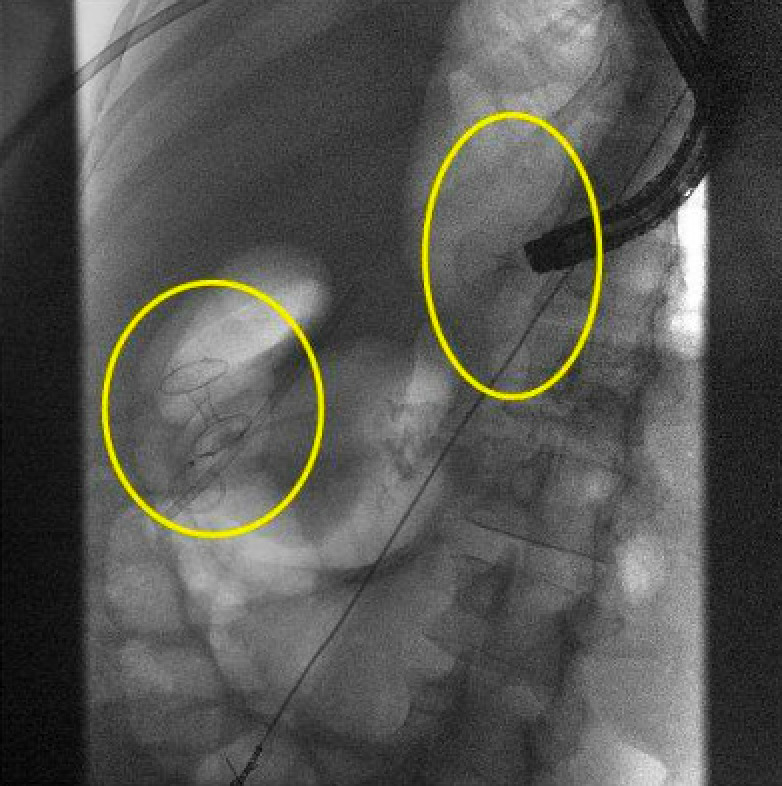
Case Description/Methods: A 37 year old woman with a past medical history of chronic pancreatitis with known pseudocysts presented to the hospital for chest and back pain associated with worsening shortness of breath. Imaging revealed a large right-sided pleural effusion and she underwent thoracentesis with chest tube placement. Fluid studies were notable for an elevated amylase level at 2,991, which raised concern for PPF in the setting of known pancreatic disease. She then underwent further evaluation with endoscopic ultrasound (EUS) and endoscopic cholangiopancreatography (ERCP). EUS showed two large pseudocysts, one in the pancreatic head and one in the body. The pancreatic head cyst had caused compression of the distal bile duct and the pancreatic body cyst likely connected with the right pleural cavity. She then underwent a biliary sphincterotomy, cyst-duodenostomy, and cystogastrostomy. Post-procedurally she experienced near-resolution of pain and shortness of breath and was discharged home with plans for outpatient follow up.
Discussion: PPFs most often occur in patients with chronic pancreatitis, and typically arise from pancreatic pseudocysts or disruption of the pancreatic duct. The pancreatic digestive enzymes result in inflammation which then causes formation of tracts from the pancreas to the pleural cavity, which can result in recurrent pleural effusions. PPF resulting in pleural effusion has been reported to occur in only 0.4% of patient’s with chronic pancreatitis, and accounts for only 1% of pleural effusion cases. This condition can be treated conservatively with administration of octreotide for exocrine suppression in addition to repeat thoracenteses, however more definitive management includes ERCP with endoscopic pancreatic stent placement and can result in substantial improvement in patient’s overall symptoms and outcome. It is important to consider this condition as a differential in patients with a known history of pancreatitis presenting with pulmonary symptoms and/or new onset pleural effusion.
Disclosures:
Hayden Rotramel, MD1, Ryan Plunkett, MD2, Ameya Deshmukh, DO2, Mahmoud Y. Madi, MD3, Wissam Kiwan, MD4. P0131 - A Rare Complication of Chronic Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1SSM Health St. Louis University Hospital, St. Louis, MO; 2Saint Louis University School of Medicine, St. Louis, MO; 3SSM Health Saint Louis University Hospital, St. Louis, MO; 4Saint Louis University, St. Louis, MO
Introduction: The formation of pancreaticopleural fistulas (PPFs) is an extremely rare complication of chronic pancreatitis. It can be difficult to diagnose this condition as patients often do not present with the typical signs or symptoms associated with pancreatitis. Here, we present a case of a woman presenting with pulmonary symptoms who was later found to have PPF secondary to chronic pancreatitis.
Case Description/Methods: A 37 year old woman with a past medical history of chronic pancreatitis with known pseudocysts presented to the hospital for chest and back pain associated with worsening shortness of breath. Imaging revealed a large right-sided pleural effusion and she underwent thoracentesis with chest tube placement. Fluid studies were notable for an elevated amylase level at 2,991, which raised concern for PPF in the setting of known pancreatic disease. She then underwent further evaluation with endoscopic ultrasound (EUS) and endoscopic cholangiopancreatography (ERCP). EUS showed two large pseudocysts, one in the pancreatic head and one in the body. The pancreatic head cyst had caused compression of the distal bile duct and the pancreatic body cyst likely connected with the right pleural cavity. She then underwent a biliary sphincterotomy, cyst-duodenostomy, and cystogastrostomy. Post-procedurally she experienced near-resolution of pain and shortness of breath and was discharged home with plans for outpatient follow up.
Discussion: PPFs most often occur in patients with chronic pancreatitis, and typically arise from pancreatic pseudocysts or disruption of the pancreatic duct. The pancreatic digestive enzymes result in inflammation which then causes formation of tracts from the pancreas to the pleural cavity, which can result in recurrent pleural effusions. PPF resulting in pleural effusion has been reported to occur in only 0.4% of patient’s with chronic pancreatitis, and accounts for only 1% of pleural effusion cases. This condition can be treated conservatively with administration of octreotide for exocrine suppression in addition to repeat thoracenteses, however more definitive management includes ERCP with endoscopic pancreatic stent placement and can result in substantial improvement in patient’s overall symptoms and outcome. It is important to consider this condition as a differential in patients with a known history of pancreatitis presenting with pulmonary symptoms and/or new onset pleural effusion.
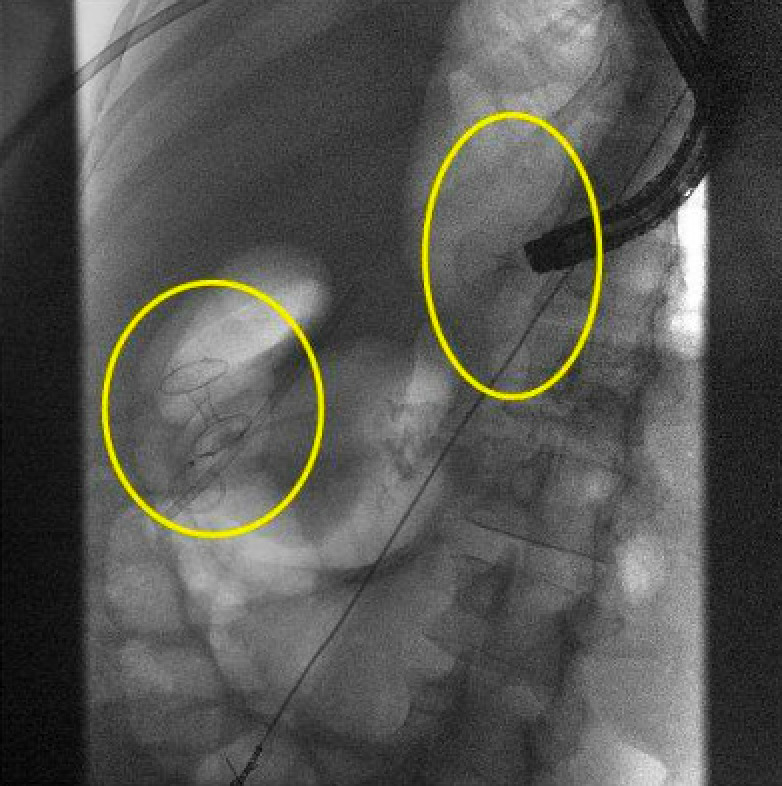
Figure: Imaging from ERCP status post cyst-duodenostomy and cystogastrostomy.
Disclosures:
Hayden Rotramel indicated no relevant financial relationships.
Ryan Plunkett indicated no relevant financial relationships.
Ameya Deshmukh indicated no relevant financial relationships.
Mahmoud Madi indicated no relevant financial relationships.
Wissam Kiwan indicated no relevant financial relationships.
Hayden Rotramel, MD1, Ryan Plunkett, MD2, Ameya Deshmukh, DO2, Mahmoud Y. Madi, MD3, Wissam Kiwan, MD4. P0131 - A Rare Complication of Chronic Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
