Sunday Poster Session
Category: Biliary/Pancreas
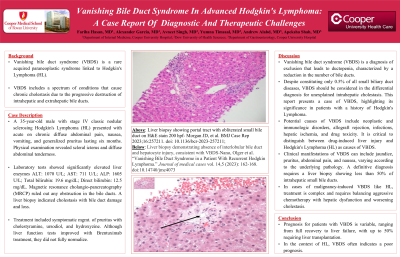
P0139 - Vanishing Bile Duct Syndrome in Advanced Hodgkin's Lymphoma: A Case Report of Diagnostic and Therapeutic Challenges
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Fariha Hasan, MD
Cooper University Hospital
Philadelphia, PA
Presenting Author(s)
Fariha Hasan, MD1, Alexander Garcia, DO2, Avneet Singh, DO2, Yumna Timsaal, MBBS3, Andrew Alabd, MD2, Apeksha Shah, MD4
1Cooper University Hospital, Philadelphia, PA; 2Cooper University Hospital, Camden, NJ; 3Dow Medical College, Karachi, Sindh, Pakistan; 4Digestive Health Institute at Cooper University Hospital, Camden, NJ
Introduction: Vanishing bile duct syndrome (VBDS) is a rare yet well-documented acquired paraneoplastic syndrome associated with Hodgkin's Lymphoma (HL). It encompasses a spectrum of conditions that result in chronic cholestasis due to the progressive destruction of intrahepatic and extrahepatic bile ducts, leading to ductopenia. In this report, we elucidate a case of VBDS, emphasizing that despite only constituting 0.5% of all small biliary duct diseases, it should be considered in the differential diagnosis for unexplained intrahepatic cholestasis in patients with a history of HL.
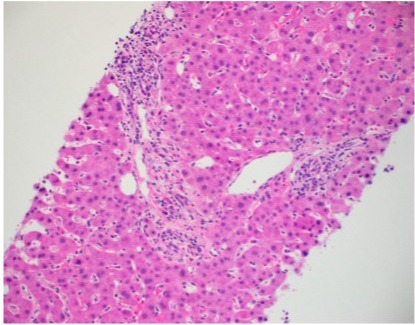
Case Description/Methods: A 35-year-old male with stage IV classic nodular sclerosing HL, non-compliant with chemotherapy, presented with acute on chronic diffuse abdominal pain, nausea, vomiting, and generalized pruritus for the past six months. Physical examination revealed scleral icterus and diffuse abdominal tenderness. Laboratory tests showed elevated liver enzymes: ALT 1070 U/L, AST 711 U/L, ALP 1605 U/L, total bilirubin 19.6 mg/dL, and direct bilirubin 12.5 mg/dL. Magnetic resonance cholangiopancreatography ruled out obstruction. A liver biopsy revealed cholestasis with bile duct damage and loss and no significant bile ductular proliferation. The patient experienced multiple hospital admissions due to abdominal pain and hepatobiliary dysfunction. Treatment included symptomatic management of pruritis, including cholestyramine, ursodiol, and hydroxyzine. While liver function tests have improved with Brentuximab, they have not fully normalized.
Discussion: VBDS is a diagnosis of exclusion, lacking specific diagnostic tests and having diverse etiologies, including neoplastic and immunologic disorders, allograft rejection, infections, hepatic ischemia, and drug toxicity. Distinguishing between drug-induced liver injury and HL as causes of VBDS is critical. Clinical manifestations such as jaundice, pruritus, abdominal pain, and nausea vary with the underlying pathology. A definitive diagnosis requires a liver biopsy demonstrating less than 50% of intrahepatic small bile ducts. Symptom management typically involves ursodeoxycholic acid and cholestyramine. In cases of malignancy-induced VBDS, such as HL, treatment is complex and necessitates balancing aggressive chemotherapy against hepatic dysfunction and worsening cholestasis. Prognosis is variable, ranging from full recovery to liver failure, with up to 50% of patients requiring liver transplantation. In the context of HL, VBDS often indicates a poor prognosis.
Disclosures:
Fariha Hasan, MD1, Alexander Garcia, DO2, Avneet Singh, DO2, Yumna Timsaal, MBBS3, Andrew Alabd, MD2, Apeksha Shah, MD4. P0139 - Vanishing Bile Duct Syndrome in Advanced Hodgkin's Lymphoma: A Case Report of Diagnostic and Therapeutic Challenges, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cooper University Hospital, Philadelphia, PA; 2Cooper University Hospital, Camden, NJ; 3Dow Medical College, Karachi, Sindh, Pakistan; 4Digestive Health Institute at Cooper University Hospital, Camden, NJ
Introduction: Vanishing bile duct syndrome (VBDS) is a rare yet well-documented acquired paraneoplastic syndrome associated with Hodgkin's Lymphoma (HL). It encompasses a spectrum of conditions that result in chronic cholestasis due to the progressive destruction of intrahepatic and extrahepatic bile ducts, leading to ductopenia. In this report, we elucidate a case of VBDS, emphasizing that despite only constituting 0.5% of all small biliary duct diseases, it should be considered in the differential diagnosis for unexplained intrahepatic cholestasis in patients with a history of HL.
Case Description/Methods: A 35-year-old male with stage IV classic nodular sclerosing HL, non-compliant with chemotherapy, presented with acute on chronic diffuse abdominal pain, nausea, vomiting, and generalized pruritus for the past six months. Physical examination revealed scleral icterus and diffuse abdominal tenderness. Laboratory tests showed elevated liver enzymes: ALT 1070 U/L, AST 711 U/L, ALP 1605 U/L, total bilirubin 19.6 mg/dL, and direct bilirubin 12.5 mg/dL. Magnetic resonance cholangiopancreatography ruled out obstruction. A liver biopsy revealed cholestasis with bile duct damage and loss and no significant bile ductular proliferation. The patient experienced multiple hospital admissions due to abdominal pain and hepatobiliary dysfunction. Treatment included symptomatic management of pruritis, including cholestyramine, ursodiol, and hydroxyzine. While liver function tests have improved with Brentuximab, they have not fully normalized.
Discussion: VBDS is a diagnosis of exclusion, lacking specific diagnostic tests and having diverse etiologies, including neoplastic and immunologic disorders, allograft rejection, infections, hepatic ischemia, and drug toxicity. Distinguishing between drug-induced liver injury and HL as causes of VBDS is critical. Clinical manifestations such as jaundice, pruritus, abdominal pain, and nausea vary with the underlying pathology. A definitive diagnosis requires a liver biopsy demonstrating less than 50% of intrahepatic small bile ducts. Symptom management typically involves ursodeoxycholic acid and cholestyramine. In cases of malignancy-induced VBDS, such as HL, treatment is complex and necessitates balancing aggressive chemotherapy against hepatic dysfunction and worsening cholestasis. Prognosis is variable, ranging from full recovery to liver failure, with up to 50% of patients requiring liver transplantation. In the context of HL, VBDS often indicates a poor prognosis.
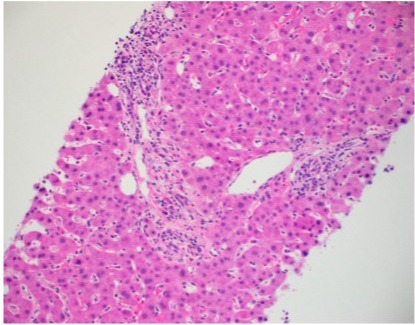
Figure: Reference photo of liver biopsy showing portal tract with obliterated small bile duct on H&E stain 200 hpf
Morgan JD, et al. BMJ Case Rep 2023;16:e257211. doi:10.1136/bcr-2023-257211
Morgan JD, et al. BMJ Case Rep 2023;16:e257211. doi:10.1136/bcr-2023-257211
Disclosures:
Fariha Hasan indicated no relevant financial relationships.
Alexander Garcia indicated no relevant financial relationships.
Avneet Singh indicated no relevant financial relationships.
Yumna Timsaal indicated no relevant financial relationships.
Andrew Alabd indicated no relevant financial relationships.
Apeksha Shah indicated no relevant financial relationships.
Fariha Hasan, MD1, Alexander Garcia, DO2, Avneet Singh, DO2, Yumna Timsaal, MBBS3, Andrew Alabd, MD2, Apeksha Shah, MD4. P0139 - Vanishing Bile Duct Syndrome in Advanced Hodgkin's Lymphoma: A Case Report of Diagnostic and Therapeutic Challenges, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
