Sunday Poster Session
Category: Biliary/Pancreas
P0141 - Pancreaticobiliary Abnormalities in a Patient With Inflammatory Bowel Disease: Looking Beyond the Obvious
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Daniyal Raza, MD
LSU Health
Shreveport, LA
Presenting Author(s)
Daniyal Raza, MD1, Alexandra E. Allman, MD2, Karan Sachdeva, MD1, Xiao Jing (Iris) Wang, MD2, Daniela Guerrero Vinsard, MD3
1LSU Health, Shreveport, LA; 2Mayo Clinic, Rochester, MN; 3University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Autoimmune pancreatitis (AIP) has two main types: type 1, also called lymphoplasmacytic sclerosing pancreatitis, and type 2, known as idiopathic duct-centric pancreatitis. Type 2 AIP can manifest in patients with inflammatory bowel disease (IBD), often linked to ulcerative colitis (UC) rather than Crohn's disease (CD). We present a case illustrating the similarity and occasional convergence between type 2 AIP and upper gastrointestinal CD, particularly with duodenal/ampullary involvement.
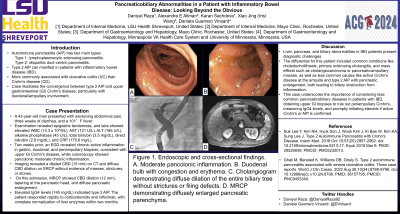
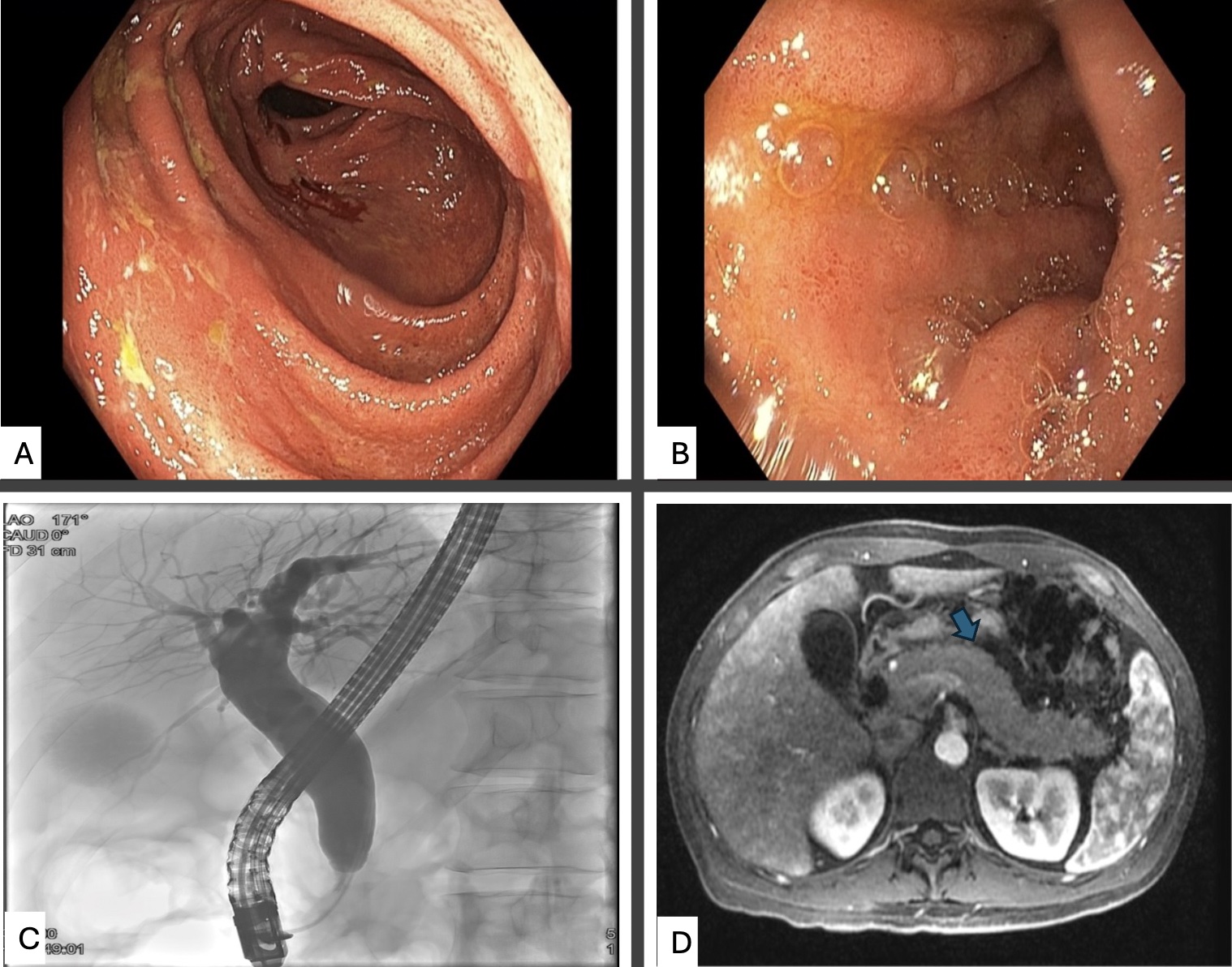
Case Description/Methods: A 43-year-old man arrived at the emergency department with worsening abdominal pain, three weeks of diarrhea, and a 101°F fever. Examination revealed only epigastric tenderness. The laboratory data were as follows: white blood cell count 13.3 x 10^9/L, aspartate aminotransferase 121 U/L, alanine aminotransferase 195 U/L, alkaline phosphatase 45 U/L, total bilirubin 3.5 mg/dL, direct bilirubin 2.8 mg/dL, and C-reactive protein 175.6 mg/L. Two weeks prior, an EGD showed chronic active inflammation in gastric, duodenal, and periampullary biopsies consistent with upper GI CD. Colonoscopy was notable for pancolonic moderate chronic inflammation. A CT scan revealed a dilated common bile duct (CBD) to 15 mm without filling defects. ERCP showed diffuse CBD dilation without an obstructive mass, strictures, or stones. On current presentation, MRCP showed CBD dilation to 12 mm despite prior sphincterotomy, along with notable CBD tapering at the pancreatic head and diffuse pancreatic enlargement. Elevated serum IgG4 (145 mg/dL) suggested type 2 AIP. The patient had a quick response to IV and oral corticosteroids along with infliximab initiation with complete normalization of liver enzymes 2 months later.
Discussion: Liver, pancreas, and biliary abnormalities in patients with IBD can pose a challenging diagnosis. The differential for our patient included common scenarios such as choledocholithiasis, primary sclerosing cholangitis, mass effect (cholangiocarcinoma, pancreatic/ampullary mass), and less common scenarios like active CD at the level of the ampulla and type 2 AIP with an enlarged pancreas, both causing biliary obstruction from inflammation. This case highlights the importance of looking beyond the most common causes of pancreaticobiliary disease when caring for patients with IBD. It is crucial to obtain biopsies of the upper GI tract to rule out periampullary Crohn’s, measure IgG4 levels, and initiate steroids timely if active CD and/or AIP are confirmed.
Disclosures:
Daniyal Raza, MD1, Alexandra E. Allman, MD2, Karan Sachdeva, MD1, Xiao Jing (Iris) Wang, MD2, Daniela Guerrero Vinsard, MD3. P0141 - Pancreaticobiliary Abnormalities in a Patient With Inflammatory Bowel Disease: Looking Beyond the Obvious, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1LSU Health, Shreveport, LA; 2Mayo Clinic, Rochester, MN; 3University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Autoimmune pancreatitis (AIP) has two main types: type 1, also called lymphoplasmacytic sclerosing pancreatitis, and type 2, known as idiopathic duct-centric pancreatitis. Type 2 AIP can manifest in patients with inflammatory bowel disease (IBD), often linked to ulcerative colitis (UC) rather than Crohn's disease (CD). We present a case illustrating the similarity and occasional convergence between type 2 AIP and upper gastrointestinal CD, particularly with duodenal/ampullary involvement.
Case Description/Methods: A 43-year-old man arrived at the emergency department with worsening abdominal pain, three weeks of diarrhea, and a 101°F fever. Examination revealed only epigastric tenderness. The laboratory data were as follows: white blood cell count 13.3 x 10^9/L, aspartate aminotransferase 121 U/L, alanine aminotransferase 195 U/L, alkaline phosphatase 45 U/L, total bilirubin 3.5 mg/dL, direct bilirubin 2.8 mg/dL, and C-reactive protein 175.6 mg/L. Two weeks prior, an EGD showed chronic active inflammation in gastric, duodenal, and periampullary biopsies consistent with upper GI CD. Colonoscopy was notable for pancolonic moderate chronic inflammation. A CT scan revealed a dilated common bile duct (CBD) to 15 mm without filling defects. ERCP showed diffuse CBD dilation without an obstructive mass, strictures, or stones. On current presentation, MRCP showed CBD dilation to 12 mm despite prior sphincterotomy, along with notable CBD tapering at the pancreatic head and diffuse pancreatic enlargement. Elevated serum IgG4 (145 mg/dL) suggested type 2 AIP. The patient had a quick response to IV and oral corticosteroids along with infliximab initiation with complete normalization of liver enzymes 2 months later.
Discussion: Liver, pancreas, and biliary abnormalities in patients with IBD can pose a challenging diagnosis. The differential for our patient included common scenarios such as choledocholithiasis, primary sclerosing cholangitis, mass effect (cholangiocarcinoma, pancreatic/ampullary mass), and less common scenarios like active CD at the level of the ampulla and type 2 AIP with an enlarged pancreas, both causing biliary obstruction from inflammation. This case highlights the importance of looking beyond the most common causes of pancreaticobiliary disease when caring for patients with IBD. It is crucial to obtain biopsies of the upper GI tract to rule out periampullary Crohn’s, measure IgG4 levels, and initiate steroids timely if active CD and/or AIP are confirmed.
Figure: Figure 1. Endoscopic and cross-sectional findings.
A. Moderate pancolonic inflammation. B. Duodenal bulb with congestion and erythema. C. Cholangiogram demonstrating diffuse dilation of the entire biliary tree without strictures or filing defects. D. MRCP demonstrating diffusely enlarged pancreatic parenchyma.
A. Moderate pancolonic inflammation. B. Duodenal bulb with congestion and erythema. C. Cholangiogram demonstrating diffuse dilation of the entire biliary tree without strictures or filing defects. D. MRCP demonstrating diffusely enlarged pancreatic parenchyma.
Disclosures:
Daniyal Raza indicated no relevant financial relationships.
Alexandra Allman indicated no relevant financial relationships.
Karan Sachdeva indicated no relevant financial relationships.
Xiao Jing (Iris) Wang indicated no relevant financial relationships.
Daniela Guerrero Vinsard indicated no relevant financial relationships.
Daniyal Raza, MD1, Alexandra E. Allman, MD2, Karan Sachdeva, MD1, Xiao Jing (Iris) Wang, MD2, Daniela Guerrero Vinsard, MD3. P0141 - Pancreaticobiliary Abnormalities in a Patient With Inflammatory Bowel Disease: Looking Beyond the Obvious, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
