Sunday Poster Session
Category: Biliary/Pancreas
P0146 - Unveiling a Rare Intersection: Secondary Syphilis Unmasking Undiagnosed Primary Biliary Cholangitis in a Male Patient
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Rakahn Haddadin, MD
MountainView Hospital
Las Vegas, NV
Presenting Author(s)
Rakahn Haddadin, MD1, Danny Aboujamra, MD2, Emon Javadi, BS3, George Trad, MD4, Homayon Iraninezhad, DO1, Pinak Shah, MD1
1MountainView Hospital, Las Vegas, NV; 2Medical University of South Carolina (MUSC) Health Florence, North York, ON, Canada; 3St. George's University School of Medicine, Anaheim Hills, CA; 4Sunrise Health GME Consortium, Las Vegas, NV
Introduction: Primary biliary cholangitis (PBC) and syphilis are both uncommon conditions, especially in male populations. Here, we present a unique case of a 43-year-old male with no significant medical history initially presenting with back and joint pain, subsequently diagnosed with both PBC and secondary syphilis.
Case Description/Methods: A 43 year old male with no significant past medical history presented to the emergency department (ED) for back and joint pain. The patient had no complaints of night sweats, chills, and denied any rash at presentation. Initial labs were significant for aspartate aminotransferase (AST) of 107 U/L , alanine aminotransferase (ALT) of 230 U/L, total bilirubin of 4.7 mg/dL, and alkaline phosphatase(ALK) of 572 U/L. A computer tomography (CT) of the abdomen showed no significant findings.
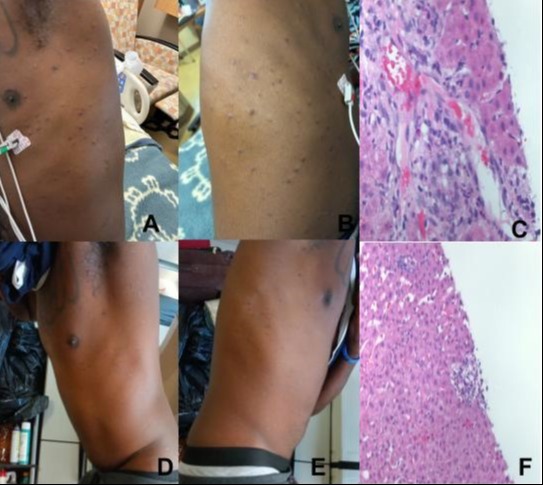
Upon further testing for the elevation in liver function tests (LFTs), the patient was found to have an elevated anti-mitochondrial antibody (AMA) of 38.2 and elevated smooth muscle IgG antibody of 27. Ursodiol was started for the patient due to meeting the criteria for PBC, with an elevated ALK >1.5 times the upper limit of normal and positive AMA. However, the patient later started to develop a rash (Figure A and Figure B). Further history obtained from the patient led to obtaining an STD panel, which showed a positive rapid plasma reagin (RPR) and positive treponemal serologic test. Treatment with doxycycline 100mg twice daily was started. Prior to discharge, the patient’s LFTs were improving.
Repeat labs in the clinic showed full resolution of the LFTs and the patient’s rash (Figure D and E) (Table 1). Liver biopsy results came back which showed liver parenchyma with a mild portal lymphocytic inflammatory infiltrate (Figures C and F). The overall features of the biopsy results were consistent with PBC.
Discussion: To our knowledge and when reviewing the literature, this is the only reported case of both confirmed PBC and secondary syphilis. There is some overlap between syphilis and PBC due to the elevated ALK and positive AMA. However, it is important to test for syphilis in these patients and consider obtaining a liver biopsy if suspicion for PBC remains high. A thorough social and sexual history should be obtained in all of these patients, along with a personal and family history of autoimmune diseases. This case highlights the need to consider PBC even in a male with no history of autoimmune disease.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Rakahn Haddadin, MD1, Danny Aboujamra, MD2, Emon Javadi, BS3, George Trad, MD4, Homayon Iraninezhad, DO1, Pinak Shah, MD1. P0146 - Unveiling a Rare Intersection: Secondary Syphilis Unmasking Undiagnosed Primary Biliary Cholangitis in a Male Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1MountainView Hospital, Las Vegas, NV; 2Medical University of South Carolina (MUSC) Health Florence, North York, ON, Canada; 3St. George's University School of Medicine, Anaheim Hills, CA; 4Sunrise Health GME Consortium, Las Vegas, NV
Introduction: Primary biliary cholangitis (PBC) and syphilis are both uncommon conditions, especially in male populations. Here, we present a unique case of a 43-year-old male with no significant medical history initially presenting with back and joint pain, subsequently diagnosed with both PBC and secondary syphilis.
Case Description/Methods: A 43 year old male with no significant past medical history presented to the emergency department (ED) for back and joint pain. The patient had no complaints of night sweats, chills, and denied any rash at presentation. Initial labs were significant for aspartate aminotransferase (AST) of 107 U/L , alanine aminotransferase (ALT) of 230 U/L, total bilirubin of 4.7 mg/dL, and alkaline phosphatase(ALK) of 572 U/L. A computer tomography (CT) of the abdomen showed no significant findings.
Upon further testing for the elevation in liver function tests (LFTs), the patient was found to have an elevated anti-mitochondrial antibody (AMA) of 38.2 and elevated smooth muscle IgG antibody of 27. Ursodiol was started for the patient due to meeting the criteria for PBC, with an elevated ALK >1.5 times the upper limit of normal and positive AMA. However, the patient later started to develop a rash (Figure A and Figure B). Further history obtained from the patient led to obtaining an STD panel, which showed a positive rapid plasma reagin (RPR) and positive treponemal serologic test. Treatment with doxycycline 100mg twice daily was started. Prior to discharge, the patient’s LFTs were improving.
Repeat labs in the clinic showed full resolution of the LFTs and the patient’s rash (Figure D and E) (Table 1). Liver biopsy results came back which showed liver parenchyma with a mild portal lymphocytic inflammatory infiltrate (Figures C and F). The overall features of the biopsy results were consistent with PBC.
Discussion: To our knowledge and when reviewing the literature, this is the only reported case of both confirmed PBC and secondary syphilis. There is some overlap between syphilis and PBC due to the elevated ALK and positive AMA. However, it is important to test for syphilis in these patients and consider obtaining a liver biopsy if suspicion for PBC remains high. A thorough social and sexual history should be obtained in all of these patients, along with a personal and family history of autoimmune diseases. This case highlights the need to consider PBC even in a male with no history of autoimmune disease.
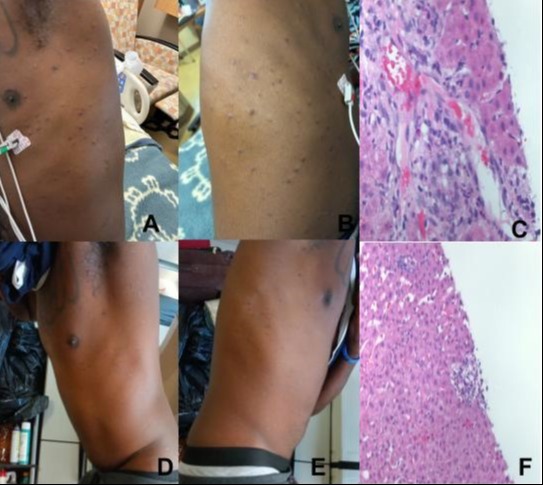
Figure: Figures: A and B - Patient's rash during hospital stay. D and E - Patient's rash at office visit. C and F - Liver biopsy results.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Rakahn Haddadin indicated no relevant financial relationships.
Danny Aboujamra indicated no relevant financial relationships.
Emon Javadi indicated no relevant financial relationships.
George Trad indicated no relevant financial relationships.
Homayon Iraninezhad indicated no relevant financial relationships.
Pinak Shah indicated no relevant financial relationships.
Rakahn Haddadin, MD1, Danny Aboujamra, MD2, Emon Javadi, BS3, George Trad, MD4, Homayon Iraninezhad, DO1, Pinak Shah, MD1. P0146 - Unveiling a Rare Intersection: Secondary Syphilis Unmasking Undiagnosed Primary Biliary Cholangitis in a Male Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
