Sunday Poster Session
Category: Biliary/Pancreas
P0170 - Expect the Unexpected: An Unusual Case of Insulinoma
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Panida Charnvitayapong, MD
University of Miami Miller School of Medicine at JFK Medical Center
Lantana, FL
Presenting Author(s)
Panida Charnvitayapong, MD1, Omar Asad, MD1, Virginia Velez-Quinones, MD2, Harrison Koss, MD2, Farrell Sheehan, MD2, Steven Soriano, DO2, Heather Wayland, MD2
1University of Miami Miller School of Medicine at JFK Medical Center, Lantana, FL; 2University of Miami Miller School of Medicine at JFK Medical Center, Atlantis, FL
Introduction: Malignant insulinomas are rare, potentially life-threatening neuroendocrine tumors that secrete excessive insulin, leading to hypoglycemia. Representing less than 10% of all insulinoma cases, they pose challenges in management and disease progression assessment. This case highlights an unusual instance of insulinoma and underscores the need for collaborative efforts to enhance knowledge and treatment strategies for this uncommon condition.
Case Description/Methods:
A 73-year-old male with no significant medical history presented with symptoms of worsening dizziness and generalized fatigue since April 2023. He experienced recurrent episodes that disrupted his daily life. He reported that during these episodes, he would drink juice or eat to return to baseline but otherwise denied any palpitations, presyncope, confusion, urinary or bowel incontinence, postural hypotension, focal neurologic deficits, abdominal pain, nausea/vomiting, change in bowel habits, and weight changes. He was referred to the hospital for further evaluation. Management of hypoglycemia required a multidisciplinary approach. Glucose levels were stabilized with IV dextrose (D5NS and D10), IM glucagon, and oral glucose tabs, with frequent adjustments. Frequent small, carbohydrate-rich meals, particularly before bedtime, and continuous glucose monitoring were implemented. Initial treatment involved carbohydrates and diazoxide, which inhibits insulin secretion from pancreatic beta cells. Our patient was initiated on diazoxide. However, diazoxide and D10 were minimally effective and caused hyponatremia, complicating the hospital course. He was transitioned to everolimus, an mTOR kinase inhibitor with antiproliferative effects, resulting in some symptom improvement before transfer to a more specialized facility. The patient still experienced occasional nocturnal hypoglycemia, but felt well overall. For patients with hepatic metastases and refractory hypoglycemia, liver-directed therapies are considered. He underwent bland hepatic artery embolization for control of liver tumor burden and was continued on everolimus, supplemented with octreotide as a combination therapy. The patient appears to be tolerating well with minimal side effects.
Discussion: Early recognition, accurate diagnosis, and a multidisciplinary approach are essential in managing hypoglycemia and controlling disease progression in malignant insulinomas. Ongoing collaboration and research are crucial for developing more effective treatment strategies for this disease.
Disclosures:
Panida Charnvitayapong, MD1, Omar Asad, MD1, Virginia Velez-Quinones, MD2, Harrison Koss, MD2, Farrell Sheehan, MD2, Steven Soriano, DO2, Heather Wayland, MD2. P0170 - Expect the Unexpected: An Unusual Case of Insulinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Miami Miller School of Medicine at JFK Medical Center, Lantana, FL; 2University of Miami Miller School of Medicine at JFK Medical Center, Atlantis, FL
Introduction: Malignant insulinomas are rare, potentially life-threatening neuroendocrine tumors that secrete excessive insulin, leading to hypoglycemia. Representing less than 10% of all insulinoma cases, they pose challenges in management and disease progression assessment. This case highlights an unusual instance of insulinoma and underscores the need for collaborative efforts to enhance knowledge and treatment strategies for this uncommon condition.
Case Description/Methods:
A 73-year-old male with no significant medical history presented with symptoms of worsening dizziness and generalized fatigue since April 2023. He experienced recurrent episodes that disrupted his daily life. He reported that during these episodes, he would drink juice or eat to return to baseline but otherwise denied any palpitations, presyncope, confusion, urinary or bowel incontinence, postural hypotension, focal neurologic deficits, abdominal pain, nausea/vomiting, change in bowel habits, and weight changes. He was referred to the hospital for further evaluation. Management of hypoglycemia required a multidisciplinary approach. Glucose levels were stabilized with IV dextrose (D5NS and D10), IM glucagon, and oral glucose tabs, with frequent adjustments. Frequent small, carbohydrate-rich meals, particularly before bedtime, and continuous glucose monitoring were implemented. Initial treatment involved carbohydrates and diazoxide, which inhibits insulin secretion from pancreatic beta cells. Our patient was initiated on diazoxide. However, diazoxide and D10 were minimally effective and caused hyponatremia, complicating the hospital course. He was transitioned to everolimus, an mTOR kinase inhibitor with antiproliferative effects, resulting in some symptom improvement before transfer to a more specialized facility. The patient still experienced occasional nocturnal hypoglycemia, but felt well overall. For patients with hepatic metastases and refractory hypoglycemia, liver-directed therapies are considered. He underwent bland hepatic artery embolization for control of liver tumor burden and was continued on everolimus, supplemented with octreotide as a combination therapy. The patient appears to be tolerating well with minimal side effects.
Discussion: Early recognition, accurate diagnosis, and a multidisciplinary approach are essential in managing hypoglycemia and controlling disease progression in malignant insulinomas. Ongoing collaboration and research are crucial for developing more effective treatment strategies for this disease.
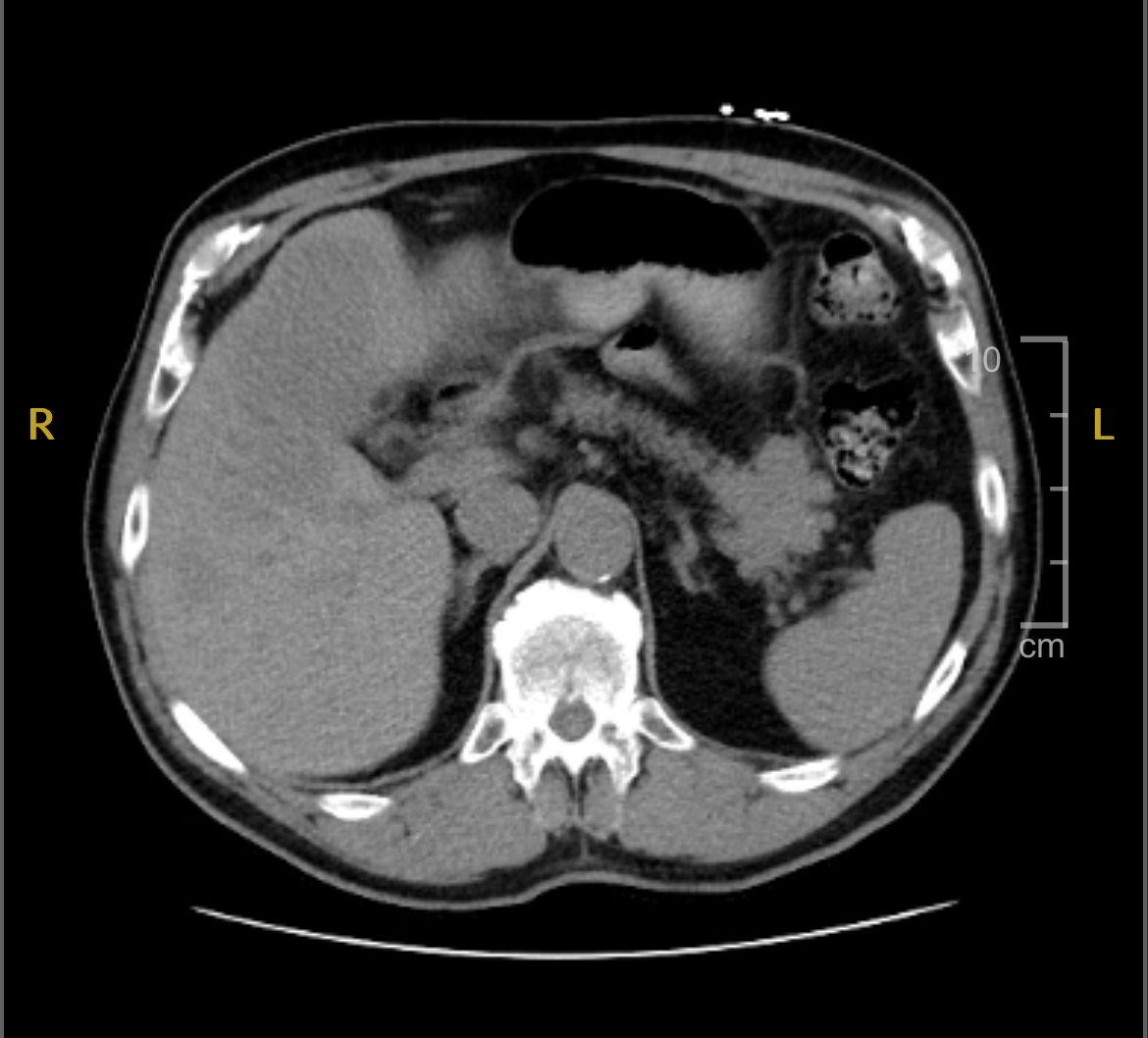
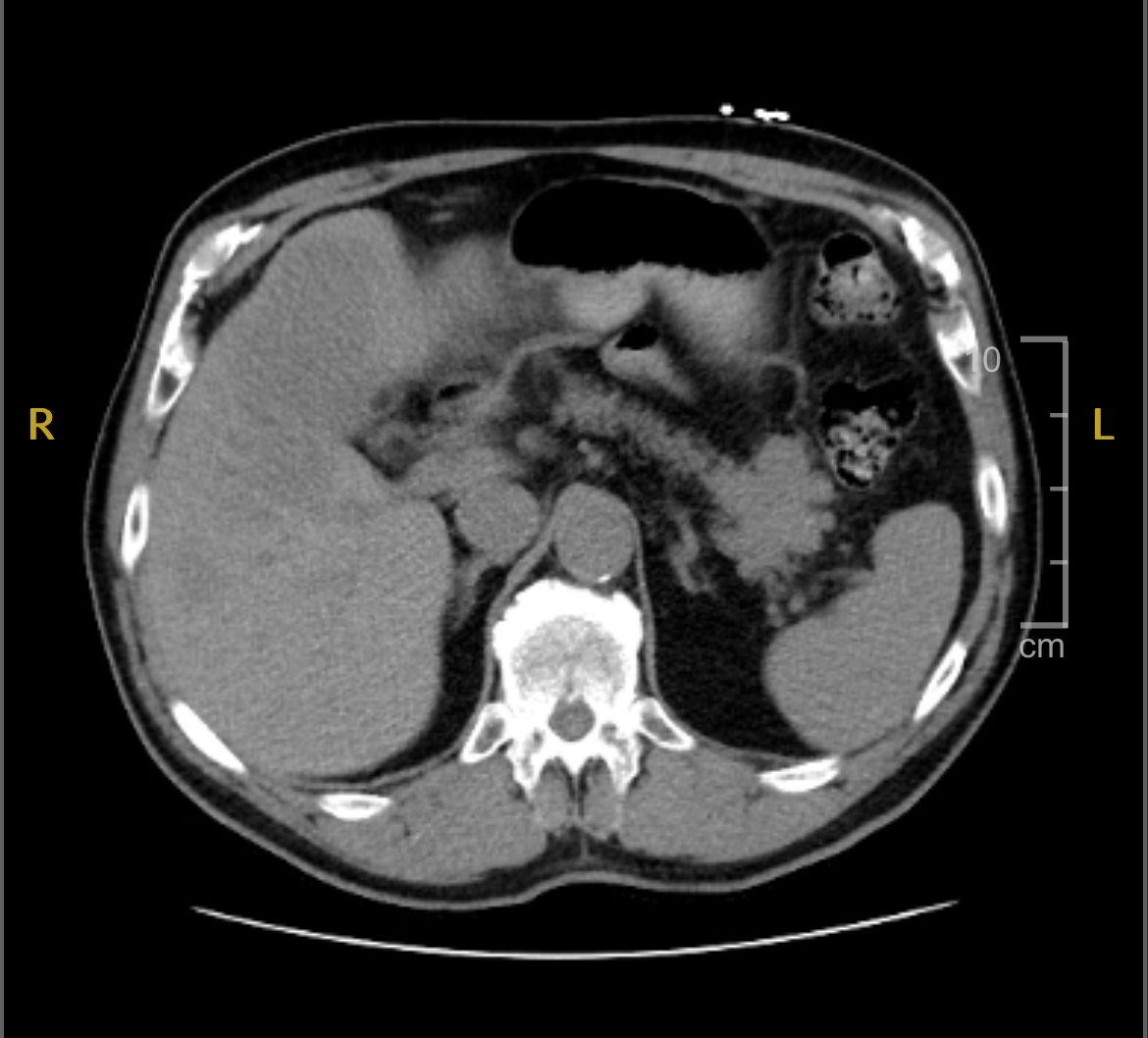
Figure: CT abdomen/pelvis of pancreatic mass
Disclosures:
Panida Charnvitayapong indicated no relevant financial relationships.
Omar Asad indicated no relevant financial relationships.
Virginia Velez-Quinones indicated no relevant financial relationships.
Harrison Koss indicated no relevant financial relationships.
Farrell Sheehan indicated no relevant financial relationships.
Steven Soriano indicated no relevant financial relationships.
Heather Wayland indicated no relevant financial relationships.
Panida Charnvitayapong, MD1, Omar Asad, MD1, Virginia Velez-Quinones, MD2, Harrison Koss, MD2, Farrell Sheehan, MD2, Steven Soriano, DO2, Heather Wayland, MD2. P0170 - Expect the Unexpected: An Unusual Case of Insulinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
