Sunday Poster Session
Category: Biliary/Pancreas
P0175 - A Rare Case of Extrahepatic Paraganglioma Presenting With Biliary Obstruction in a 29-Year-Old Male
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Irhoboudu D. Atogwe, MD
Albert Einstein Medical Center
Philadelphia, PA
Presenting Author(s)
Irhoboudu D. Atogwe, MD1, Maria Lagarde Mussa, MD2, Lisa Barrett, DO1, Blanche Echikunwoke, MBBS1, Olubunmi Shoyele, MD3
1Albert Einstein Medical Center, Philadelphia, PA; 2Einstein Medical Center, Philadelphia, PA; 3Einstein Healthcare Network, Philadelphia, PA
Introduction: Paragangliomas represent uncommon neuroendocrine tumors originating from extra-adrenal autonomic paraganglia, primarily comprised of neuroendocrine cells capable of catecholamine secretion.
Paragangliomas are a rare etiology of biliary obstruction. Although up to 55% of sympathetic paragangliomas arise in the abdomen, extrinsic compression of the biliary tree is exceptionally rare.
Case Description/Methods: A 29-year-old male with a past medical history of ankylosing spondylitis presented to the clinic for evaluation of ALT levels, accompanied by mild elevations in alkaline phosphatase and AST levels. Serological tests for autoimmune, infectious, drug induced, and other potential causes of liver disease were all negative.
A liver ultrasound revealed several mass-like lesions throughout the right hepatic lobe exerting mass effect on the porta hepatis with development of varices. A subsequent MRI confirmed an external mass likely lymphoproliferative in origin, exerting pressure on the mid common bile duct with intra and extrahepatic biliary ductal dilatation. Notably, no morphological indications of cirrhosis or intraparenchymal liver lesions were observed.
An endoscopic ultrasound (EUS) showed an 11mm dilation of the common hepatic duct and a mass that was not amenable to biopsy due to increased surrounding vascularity. Endoscopic retrograde cholangiopancreatography (ERCP) showed a localized 10mm stenotic area of the main bile duct. Liver function test normalized following stent placement. An esophagogastroduodenoscopy (EGD) showed duodenal, gastroesophageal and isolated gastric varices that did not require banding.
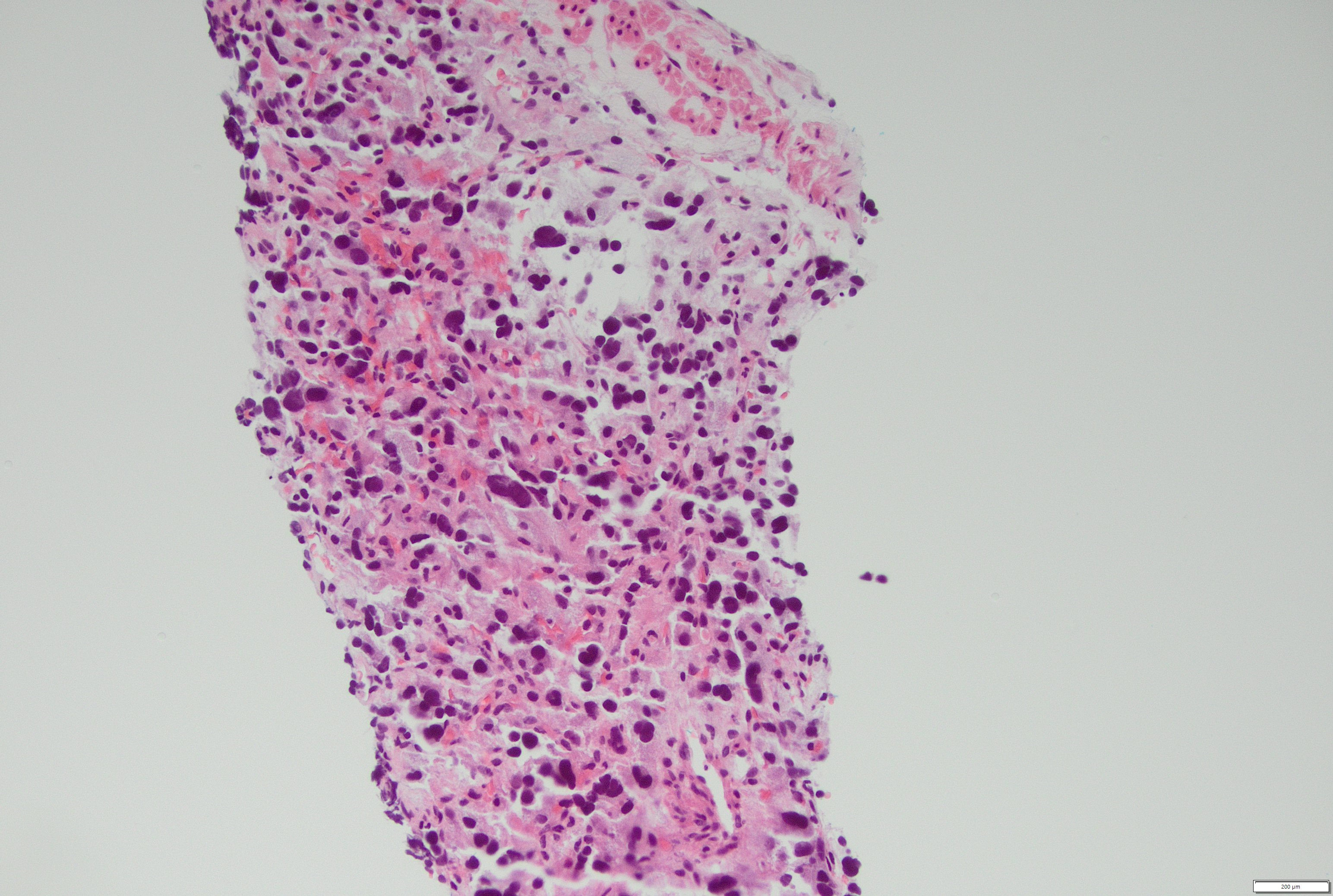
Interventional radiology performed a biopsy of the periportal mass, which turned out to be positive for synaptophysin, chromogranin and GATA-3 indicating an extrahepatic paraganglioma. Given the lesion's high vascularity, surgical intervention was deemed challenging, leading to the decision to pursue portal vein stenting temporarily with plans for eventual surgery.
Discussion: Our case highlights the infrequent occurrence of extrahepatic paragangliomas causing obstruction of the biliary tree. Predominantly originating from retroperitoneal paraganglia along the abdominal aorta, these masses are closely associated with the sympathetic nervous system and are known for catecholamine secretion. Biliary tree involvement is exceedingly rare. This is a rare condition and should always be considered in the differential of abdominal masses.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Irhoboudu D. Atogwe, MD1, Maria Lagarde Mussa, MD2, Lisa Barrett, DO1, Blanche Echikunwoke, MBBS1, Olubunmi Shoyele, MD3. P0175 - A Rare Case of Extrahepatic Paraganglioma Presenting With Biliary Obstruction in a 29-Year-Old Male, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Albert Einstein Medical Center, Philadelphia, PA; 2Einstein Medical Center, Philadelphia, PA; 3Einstein Healthcare Network, Philadelphia, PA
Introduction: Paragangliomas represent uncommon neuroendocrine tumors originating from extra-adrenal autonomic paraganglia, primarily comprised of neuroendocrine cells capable of catecholamine secretion.
Paragangliomas are a rare etiology of biliary obstruction. Although up to 55% of sympathetic paragangliomas arise in the abdomen, extrinsic compression of the biliary tree is exceptionally rare.
Case Description/Methods: A 29-year-old male with a past medical history of ankylosing spondylitis presented to the clinic for evaluation of ALT levels, accompanied by mild elevations in alkaline phosphatase and AST levels. Serological tests for autoimmune, infectious, drug induced, and other potential causes of liver disease were all negative.
A liver ultrasound revealed several mass-like lesions throughout the right hepatic lobe exerting mass effect on the porta hepatis with development of varices. A subsequent MRI confirmed an external mass likely lymphoproliferative in origin, exerting pressure on the mid common bile duct with intra and extrahepatic biliary ductal dilatation. Notably, no morphological indications of cirrhosis or intraparenchymal liver lesions were observed.
An endoscopic ultrasound (EUS) showed an 11mm dilation of the common hepatic duct and a mass that was not amenable to biopsy due to increased surrounding vascularity. Endoscopic retrograde cholangiopancreatography (ERCP) showed a localized 10mm stenotic area of the main bile duct. Liver function test normalized following stent placement. An esophagogastroduodenoscopy (EGD) showed duodenal, gastroesophageal and isolated gastric varices that did not require banding.
Interventional radiology performed a biopsy of the periportal mass, which turned out to be positive for synaptophysin, chromogranin and GATA-3 indicating an extrahepatic paraganglioma. Given the lesion's high vascularity, surgical intervention was deemed challenging, leading to the decision to pursue portal vein stenting temporarily with plans for eventual surgery.
Discussion: Our case highlights the infrequent occurrence of extrahepatic paragangliomas causing obstruction of the biliary tree. Predominantly originating from retroperitoneal paraganglia along the abdominal aorta, these masses are closely associated with the sympathetic nervous system and are known for catecholamine secretion. Biliary tree involvement is exceedingly rare. This is a rare condition and should always be considered in the differential of abdominal masses.
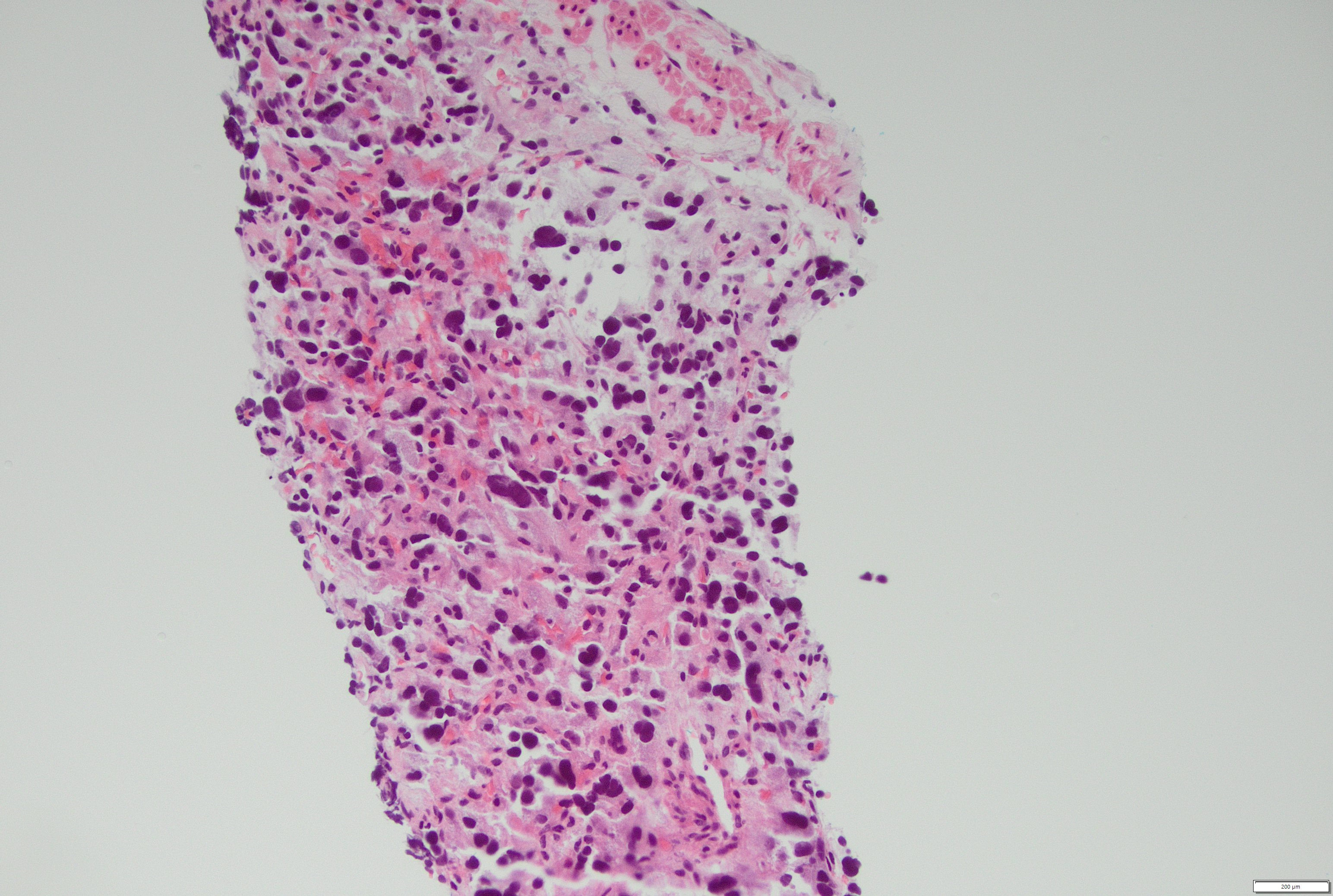
Figure: Periportal mass biopsy (H&E) showing epithelioid cells with eosinophilic cytoplasm, focal nuclear pleomorphism, and nuclear hyperchromasia
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Irhoboudu Atogwe indicated no relevant financial relationships.
Maria Lagarde Mussa indicated no relevant financial relationships.
Lisa Barrett indicated no relevant financial relationships.
Blanche Echikunwoke indicated no relevant financial relationships.
Olubunmi Shoyele indicated no relevant financial relationships.
Irhoboudu D. Atogwe, MD1, Maria Lagarde Mussa, MD2, Lisa Barrett, DO1, Blanche Echikunwoke, MBBS1, Olubunmi Shoyele, MD3. P0175 - A Rare Case of Extrahepatic Paraganglioma Presenting With Biliary Obstruction in a 29-Year-Old Male, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
