Sunday Poster Session
Category: Biliary/Pancreas
P0181 - Endoscopic Papillectomy for a Rare Case of Synchronous Major and Minor Papillary Adenoma
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
Hossein Haghbin, MD, MPH
Ascension Providence Hospital
Novi, MI
Presenting Author(s)
Hossein Haghbin, MD, MPH1, Reshad Salam, MD2, Edward Yousif, MD2, Roberto Gamarra, MD2
1Ascension Providence Hospital, Novi, MI; 2Ascension Providence Hospital, Southfield, MI
Introduction: Adenoma of ampulla of Vater can occur sporadically or with risk factor of familial adenomatous polyposis (FAP) syndrome. Exceedingly rare is the endoscopic resection of simultaneous occurrence of adenoma in both papillae with only two prior cases reported in literature, both in adenomatous polyposis syndromes. We present the first case of endoscopic resection of major and minor papillae in a patient with no prior FAP.
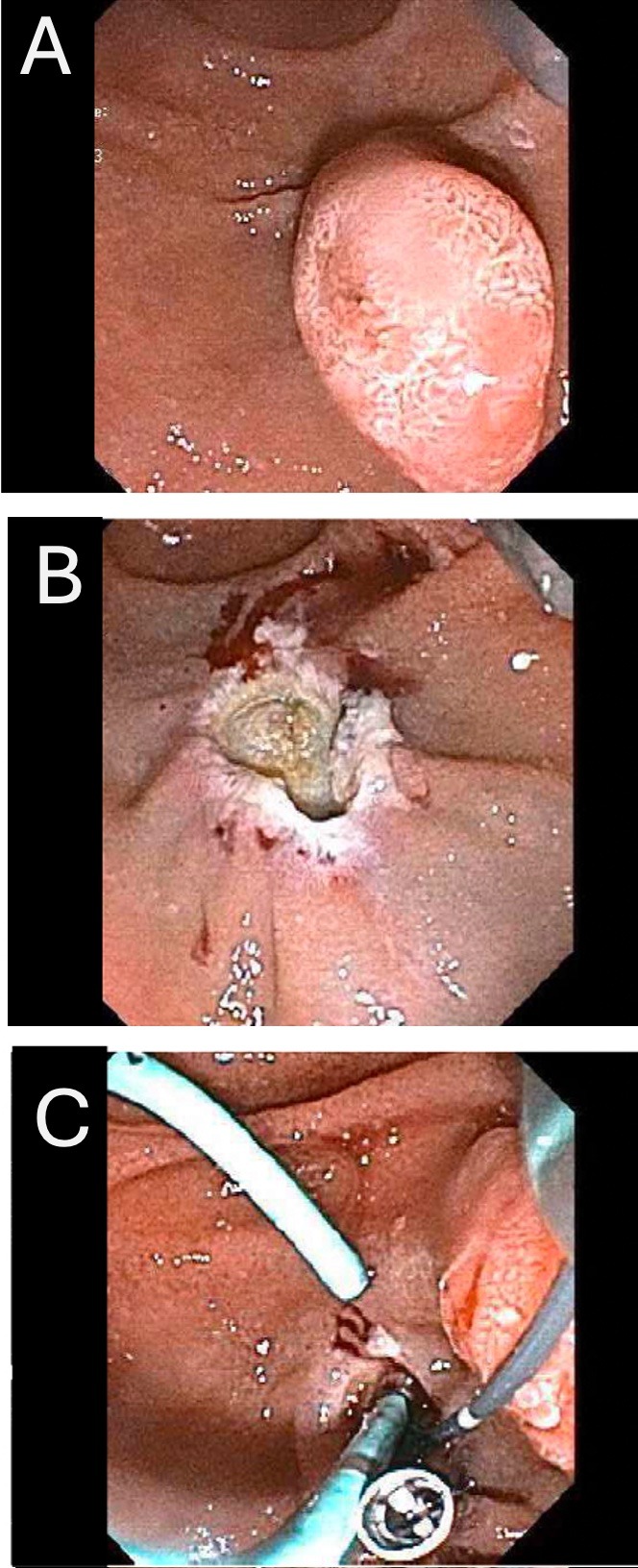
Case Description/Methods: A 74-year-old lady was referred for evaluation and resection of incidentally found adenoma of minor and major papilla during upper endoscopy. Subsequent EUS showed that the adenomas were limited to deep mucosa (layer 2) and histopathology results confirmed adenoma with no high-grade dysplasia; therefore, she was scheduled for endoscopic papillectomy. Endoscopic retrograde pancreatography (ERCP) with sphincterotomy and stenting of both ventral pancreatic duct (PD) and common bile duct was performed. The submucosa of the major papillae was lifted with solution containing normal saline, 1:10,000 epinephrine, and methylene blue. We performed hot snare papillectomy followed by hot forceps ablation of margins and any visualized residual tissue. In follow-up ERCP, we performed minor papillectomy with dorsal PD stent insertion. Follow up surveillance in three months indicated no recurrence in either major or minor papillae. Patient is currently scheduled for surveillance in one year.
Discussion: Endoscopic resection of simultaneous occurrence of major and minor papilla adenoma is exceedingly rare with this case being the first endoscopic papillectomy of both papillae in a patient with no adenomatous polyposis syndrome in herself or in any of her first-degree relatives. In this patient, EUS ruled out invasion to deep submucosa and muscularis propria; hence, she was amenable to endoscopic intervention. Endoscopic papillectomy is a safe procedure, however recurrence rates can be as high as 1 in 3, especially in cases of piecemeal resection. Therefore, follow up endoscopic surveillance is recommended. After papillectomy, we used hot forceps for both ablation of any residual tissue and for thermo-ablation of the margins to reduce recurrence rates. Pancreatic stent to either ventral or dorsal PD was inserted to minimize risk of post ERCP pancreatitis and stenosis of the pancreatic orifice which were avoided in this patient. Due to no definite recurrence in the 3-month surveillance endoscopy, continuing surveillance in one year is appropriate.
Disclosures:
Hossein Haghbin, MD, MPH1, Reshad Salam, MD2, Edward Yousif, MD2, Roberto Gamarra, MD2. P0181 - Endoscopic Papillectomy for a Rare Case of Synchronous Major and Minor Papillary Adenoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Ascension Providence Hospital, Novi, MI; 2Ascension Providence Hospital, Southfield, MI
Introduction: Adenoma of ampulla of Vater can occur sporadically or with risk factor of familial adenomatous polyposis (FAP) syndrome. Exceedingly rare is the endoscopic resection of simultaneous occurrence of adenoma in both papillae with only two prior cases reported in literature, both in adenomatous polyposis syndromes. We present the first case of endoscopic resection of major and minor papillae in a patient with no prior FAP.
Case Description/Methods: A 74-year-old lady was referred for evaluation and resection of incidentally found adenoma of minor and major papilla during upper endoscopy. Subsequent EUS showed that the adenomas were limited to deep mucosa (layer 2) and histopathology results confirmed adenoma with no high-grade dysplasia; therefore, she was scheduled for endoscopic papillectomy. Endoscopic retrograde pancreatography (ERCP) with sphincterotomy and stenting of both ventral pancreatic duct (PD) and common bile duct was performed. The submucosa of the major papillae was lifted with solution containing normal saline, 1:10,000 epinephrine, and methylene blue. We performed hot snare papillectomy followed by hot forceps ablation of margins and any visualized residual tissue. In follow-up ERCP, we performed minor papillectomy with dorsal PD stent insertion. Follow up surveillance in three months indicated no recurrence in either major or minor papillae. Patient is currently scheduled for surveillance in one year.
Discussion: Endoscopic resection of simultaneous occurrence of major and minor papilla adenoma is exceedingly rare with this case being the first endoscopic papillectomy of both papillae in a patient with no adenomatous polyposis syndrome in herself or in any of her first-degree relatives. In this patient, EUS ruled out invasion to deep submucosa and muscularis propria; hence, she was amenable to endoscopic intervention. Endoscopic papillectomy is a safe procedure, however recurrence rates can be as high as 1 in 3, especially in cases of piecemeal resection. Therefore, follow up endoscopic surveillance is recommended. After papillectomy, we used hot forceps for both ablation of any residual tissue and for thermo-ablation of the margins to reduce recurrence rates. Pancreatic stent to either ventral or dorsal PD was inserted to minimize risk of post ERCP pancreatitis and stenosis of the pancreatic orifice which were avoided in this patient. Due to no definite recurrence in the 3-month surveillance endoscopy, continuing surveillance in one year is appropriate.
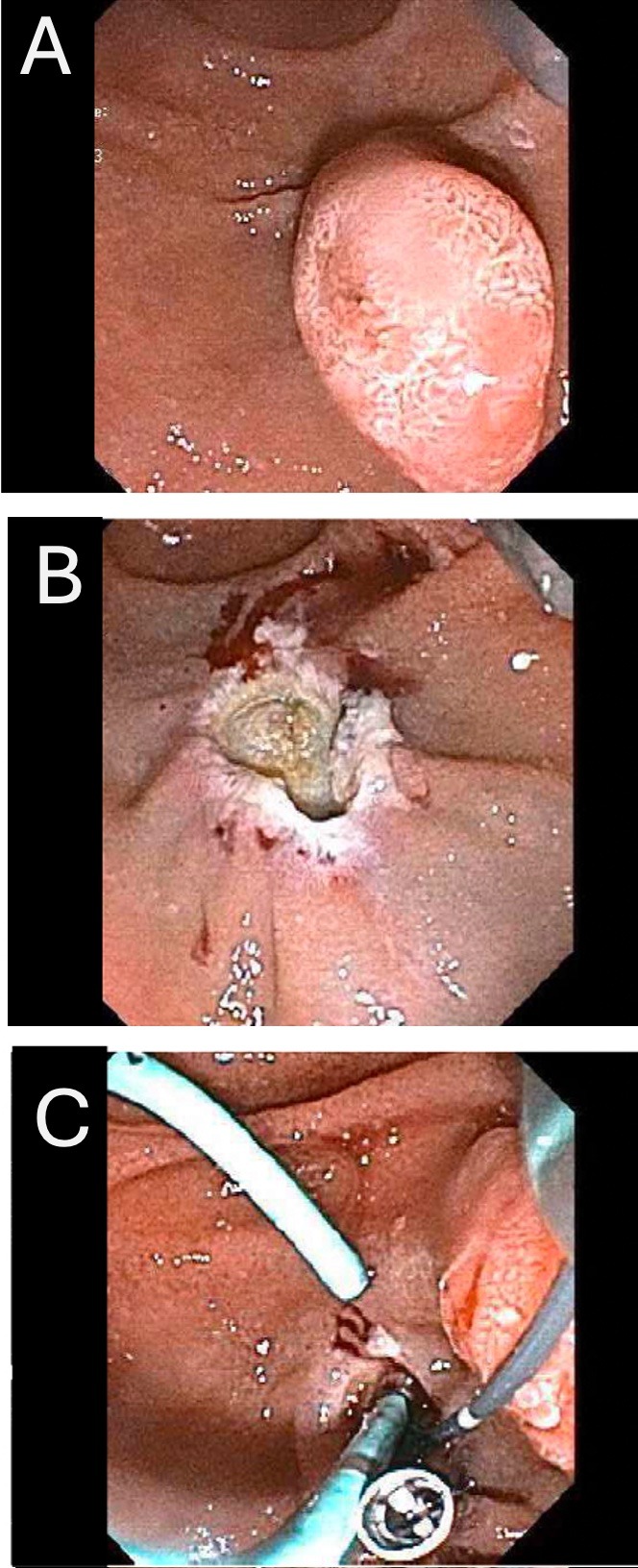
Figure: Endoscopic papillectomy for ampullary adenoma with stent insertion and clipping.
Disclosures:
Hossein Haghbin indicated no relevant financial relationships.
Reshad Salam indicated no relevant financial relationships.
Edward Yousif indicated no relevant financial relationships.
Roberto Gamarra indicated no relevant financial relationships.
Hossein Haghbin, MD, MPH1, Reshad Salam, MD2, Edward Yousif, MD2, Roberto Gamarra, MD2. P0181 - Endoscopic Papillectomy for a Rare Case of Synchronous Major and Minor Papillary Adenoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
