Sunday Poster Session
Category: Colon
P0204 - Demographic and Socioeconomic Disparities in the Co-Occurrence of Clostridioides Difficile Infection and Chronic Kidney Disease – A Population-Based Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Ritik M. Goyal, MBBS
Rutgers New Jersey Medical School
Newark, NJ
Presenting Author(s)
Ritik M. Goyal, MBBS1, Sameer Rao, MBBS2, Anmol Mittal, MD1, Mohamed Ismail, DO1, Wajiha Khan, MD3, Kranthi Mandava, MD1, Imran A. Qureshi, MD1, Ahmed Al-Khazraji, MD1
1Rutgers New Jersey Medical School, Newark, NJ; 2Mayo Clinic, Rochester, MN; 3Rutgers New Jersey Medical School, Cartaret, NJ
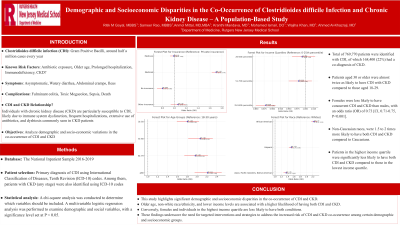
Introduction: Clostridioides difficile infection (CDI) is a prevalent cause of diarrhea, with its incidence rising over time. Individuals with chronic kidney disease (CKD) are particularly susceptible to CDI, likely due to immune system dysfunction, frequent hospitalizations, extensive use of antibiotics, and dysbiosis commonly seen in CKD patients. This study aims to analyze demographic and socio-economic variations in the co-occurrence of CDI and CKD.
Methods: The National Inpatient Sample (NIS) database from 2016-2019 was queried to identify patients with a primary diagnosis of CDI using International Classification of Diseases, Tenth Revision (ICD-10) codes. Among them, patients with CKD (any stage) were also identified using ICD-10 codes. A chi-square analysis was conducted to determine which variables should be included. A multivariable logistic regression analysis was performed to examine demographic and social variables, with a significance level set at P < 0.05.
Results: A total of 769,770 patients were identified with CDI, of which 168,400 (22%) had a co-diagnosis of chronic kidney disease. Patients aged 30 or older were almost twice as likely to have CDI with CKD compared to those aged 18-29. Females were less likely to have concurrent CDI and CKD than males, with an odds ratio (OR) of 0.73 [CI, 0.71-0.75, P< 0.001]. Non-Caucasian races, including African Americans, Asians, Pacific Islanders, Native Americans, and Hispanics, were 1.5 to 2 times more likely to have both CDI and CKD compared to Caucasians. Patients in the highest income quartile (76-100%) were significantly less likely to have both CDI and CKD compared to those in the lowest income quartile (0-25%), with an OR of 0.88 [CI, 0.85-0.91, P < 0.001]. Compared to those with private insurance, patients with Medicaid were 1.7 times more likely to have both CDI and CKD, whereas uninsured patients were less likely to have both conditions, with an OR of 0.80 [CI, 0.71-0.90, P < 0.001].
Discussion: This study highlights significant demographic and socioeconomic disparities in the co-occurrence of CDI and CKD. Older age, non-white race/ethnicity, and lower income levels are associated with a higher likelihood of having both CDI and CKD. Conversely, females and individuals in the highest income quartile are less likely to have both conditions. These findings underscore the need for targeted interventions and strategies to address the increased risk of CDI and CKD co-occurrence among certain demographic and socioeconomic groups.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ritik M. Goyal, MBBS1, Sameer Rao, MBBS2, Anmol Mittal, MD1, Mohamed Ismail, DO1, Wajiha Khan, MD3, Kranthi Mandava, MD1, Imran A. Qureshi, MD1, Ahmed Al-Khazraji, MD1. P0204 - Demographic and Socioeconomic Disparities in the Co-Occurrence of Clostridioides Difficile Infection and Chronic Kidney Disease – A Population-Based Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Rutgers New Jersey Medical School, Newark, NJ; 2Mayo Clinic, Rochester, MN; 3Rutgers New Jersey Medical School, Cartaret, NJ
Introduction: Clostridioides difficile infection (CDI) is a prevalent cause of diarrhea, with its incidence rising over time. Individuals with chronic kidney disease (CKD) are particularly susceptible to CDI, likely due to immune system dysfunction, frequent hospitalizations, extensive use of antibiotics, and dysbiosis commonly seen in CKD patients. This study aims to analyze demographic and socio-economic variations in the co-occurrence of CDI and CKD.
Methods: The National Inpatient Sample (NIS) database from 2016-2019 was queried to identify patients with a primary diagnosis of CDI using International Classification of Diseases, Tenth Revision (ICD-10) codes. Among them, patients with CKD (any stage) were also identified using ICD-10 codes. A chi-square analysis was conducted to determine which variables should be included. A multivariable logistic regression analysis was performed to examine demographic and social variables, with a significance level set at P < 0.05.
Results: A total of 769,770 patients were identified with CDI, of which 168,400 (22%) had a co-diagnosis of chronic kidney disease. Patients aged 30 or older were almost twice as likely to have CDI with CKD compared to those aged 18-29. Females were less likely to have concurrent CDI and CKD than males, with an odds ratio (OR) of 0.73 [CI, 0.71-0.75, P< 0.001]. Non-Caucasian races, including African Americans, Asians, Pacific Islanders, Native Americans, and Hispanics, were 1.5 to 2 times more likely to have both CDI and CKD compared to Caucasians. Patients in the highest income quartile (76-100%) were significantly less likely to have both CDI and CKD compared to those in the lowest income quartile (0-25%), with an OR of 0.88 [CI, 0.85-0.91, P < 0.001]. Compared to those with private insurance, patients with Medicaid were 1.7 times more likely to have both CDI and CKD, whereas uninsured patients were less likely to have both conditions, with an OR of 0.80 [CI, 0.71-0.90, P < 0.001].
Discussion: This study highlights significant demographic and socioeconomic disparities in the co-occurrence of CDI and CKD. Older age, non-white race/ethnicity, and lower income levels are associated with a higher likelihood of having both CDI and CKD. Conversely, females and individuals in the highest income quartile are less likely to have both conditions. These findings underscore the need for targeted interventions and strategies to address the increased risk of CDI and CKD co-occurrence among certain demographic and socioeconomic groups.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ritik Goyal indicated no relevant financial relationships.
Sameer Rao indicated no relevant financial relationships.
Anmol Mittal indicated no relevant financial relationships.
Mohamed Ismail indicated no relevant financial relationships.
Wajiha Khan indicated no relevant financial relationships.
Kranthi Mandava indicated no relevant financial relationships.
Imran Qureshi indicated no relevant financial relationships.
Ahmed Al-Khazraji indicated no relevant financial relationships.
Ritik M. Goyal, MBBS1, Sameer Rao, MBBS2, Anmol Mittal, MD1, Mohamed Ismail, DO1, Wajiha Khan, MD3, Kranthi Mandava, MD1, Imran A. Qureshi, MD1, Ahmed Al-Khazraji, MD1. P0204 - Demographic and Socioeconomic Disparities in the Co-Occurrence of Clostridioides Difficile Infection and Chronic Kidney Disease – A Population-Based Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
