Sunday Poster Session
Category: Colon
P0239 - Non-Neoplastic Polyp Detection Using AI, GI Genius, With Experienced Endoscopist - Pilot Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- WR
Warman Roshan, BA
University of South Florida
Philadelphia, PA
Presenting Author(s)
Roshan Warman, BA1, Tanush Singh, 2, Jose lezama, MD3, Julia E. Gallagher, BA4, Andrew Borkowski, MD3, Gitanjali Vidyarthi, MD3
1University of South Florida, Philadelphia, PA; 2James A. Haley Veterans' Hospital, Orange City, NJ; 3James A. Haley Veterans' Hospital, Tampa, FL; 4University of South Florida, Tampa, FL
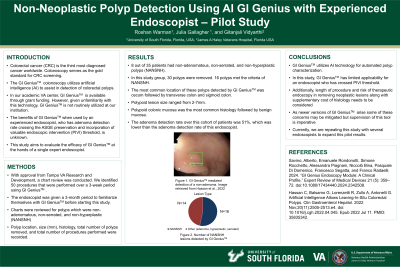
Introduction: GI genius leverages cutting edge algorithms and numerous publications on its efficacy has led to its integration in many clinical practices. In addition to detecting polyps, it has also been shown to accelerate the learning of fellows in endoscopy suites. In our academic VA center, it is available through a Grant. As it gets embedded in daily usage the cost is likely to increase. Given unfamiliarity with this new technology, assumed unclear benefits many endoscopists are hesitant to use it.. Furthermore, the benefits in the hands of experienced endoscopist with adenoma detection rate crossing the ASGE's preservation and incorporation of valuable endoscopic intervention (PIVI) threshold is unknown. Thus, this study was undertaken to evaluate the efficacy of GI Genius at the hands of a single expert endoscopist.
Methods: Methods -after getting the IRB approval, chart was reviewed for 50 procedures done over a 3-week using GI genius. A 3-month period was given to get accustomed to GI genius before starting this study. Chart was reviewed for polyps which were non-adenomatous non-serrated and non-hyperplastic (NANSNH). The location of polyps, size, histology, total number of polyps removed on each of those days along with total number of procedures performed were noted.
Results: Results – 8 out of 35 patients had non-adenomatous non-serrated and non-hyperplastic polys detected by GI Genius. In this study group 30 polyps were removed out of which 16 met the criteria of NANSNH. The most common location of these polyps as detected by GI-Genius was cecum followed by transverse colon and sigmoid colon. The size of these polypoid lesions ranged from 2 mm to 7mm, and the most common histology was polypoid colonic mucosa followed by benign mucosa. The adenoma detection rate over this cohort of patients was lower than historic adenoma detection rate of this endoscopist.
Discussion: Conclusion - GI genius designed for automated polyp characterization has limited applicability in endoscopists who have crossed PIVI threshold. Additionally, increased length of procedure, adding risk of therapeutic endoscopy in removing nonneoplastic lesions along with supplementary cost of histology needs to be considered. As newer versions of GI genius will come along and some of this may be mitigated but supervision over this tool is imperative as experts endoscopist have the responsibility to shape the future of endoscopy. At this time we are doing this study over several endoscopists to expand on this pilot result.
Disclosures:
Roshan Warman, BA1, Tanush Singh, 2, Jose lezama, MD3, Julia E. Gallagher, BA4, Andrew Borkowski, MD3, Gitanjali Vidyarthi, MD3. P0239 - Non-Neoplastic Polyp Detection Using AI, GI Genius, With Experienced Endoscopist - Pilot Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of South Florida, Philadelphia, PA; 2James A. Haley Veterans' Hospital, Orange City, NJ; 3James A. Haley Veterans' Hospital, Tampa, FL; 4University of South Florida, Tampa, FL
Introduction: GI genius leverages cutting edge algorithms and numerous publications on its efficacy has led to its integration in many clinical practices. In addition to detecting polyps, it has also been shown to accelerate the learning of fellows in endoscopy suites. In our academic VA center, it is available through a Grant. As it gets embedded in daily usage the cost is likely to increase. Given unfamiliarity with this new technology, assumed unclear benefits many endoscopists are hesitant to use it.. Furthermore, the benefits in the hands of experienced endoscopist with adenoma detection rate crossing the ASGE's preservation and incorporation of valuable endoscopic intervention (PIVI) threshold is unknown. Thus, this study was undertaken to evaluate the efficacy of GI Genius at the hands of a single expert endoscopist.
Methods: Methods -after getting the IRB approval, chart was reviewed for 50 procedures done over a 3-week using GI genius. A 3-month period was given to get accustomed to GI genius before starting this study. Chart was reviewed for polyps which were non-adenomatous non-serrated and non-hyperplastic (NANSNH). The location of polyps, size, histology, total number of polyps removed on each of those days along with total number of procedures performed were noted.
Results: Results – 8 out of 35 patients had non-adenomatous non-serrated and non-hyperplastic polys detected by GI Genius. In this study group 30 polyps were removed out of which 16 met the criteria of NANSNH. The most common location of these polyps as detected by GI-Genius was cecum followed by transverse colon and sigmoid colon. The size of these polypoid lesions ranged from 2 mm to 7mm, and the most common histology was polypoid colonic mucosa followed by benign mucosa. The adenoma detection rate over this cohort of patients was lower than historic adenoma detection rate of this endoscopist.
Discussion: Conclusion - GI genius designed for automated polyp characterization has limited applicability in endoscopists who have crossed PIVI threshold. Additionally, increased length of procedure, adding risk of therapeutic endoscopy in removing nonneoplastic lesions along with supplementary cost of histology needs to be considered. As newer versions of GI genius will come along and some of this may be mitigated but supervision over this tool is imperative as experts endoscopist have the responsibility to shape the future of endoscopy. At this time we are doing this study over several endoscopists to expand on this pilot result.
Disclosures:
Roshan Warman indicated no relevant financial relationships.
Tanush Singh indicated no relevant financial relationships.
Jose lezama indicated no relevant financial relationships.
Julia Gallagher indicated no relevant financial relationships.
Andrew Borkowski indicated no relevant financial relationships.
Gitanjali Vidyarthi indicated no relevant financial relationships.
Roshan Warman, BA1, Tanush Singh, 2, Jose lezama, MD3, Julia E. Gallagher, BA4, Andrew Borkowski, MD3, Gitanjali Vidyarthi, MD3. P0239 - Non-Neoplastic Polyp Detection Using AI, GI Genius, With Experienced Endoscopist - Pilot Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
