Sunday Poster Session
Category: Colon
P0247 - Contemporary Nationwide Trends and Predictors of Venous Thromboembolism and Mortality in Elderly Asian American and Pacific Islander Patients Hospitalized With Colorectal Cancer: A Comprehensive Analysis (2016-2020)
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Azra Kothawala, MBBS
Jawaharlal Nehru Medical College
Belgaum, Karnataka, India
Presenting Author(s)
Azra Kothawala, MBBS1, Asees Lubana, 2, Anisha Chhabra, 2, Shreya Madan, 2, Rupak Desai, MBBS3
1Jawaharlal Nehru Medical College, Belgaum, Karnataka, India; 2Desert Mountain High School, Scottsdale, AZ; 3Outcomes Research, Atlanta, GA
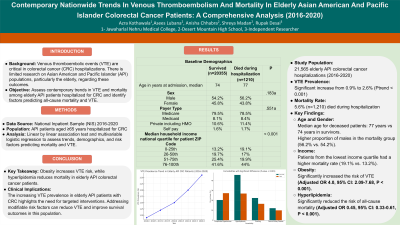
Introduction: Venous thromboembolic events (VTE) and associated mortality are critical concerns in colorectal cancer (CRC) hospitalizations. The Asian American and Pacific Islander (API) elderly population is understudied in this context. This study assesses contemporary trends in VTE and mortality among elderly API patients hospitalized for CRC. It seeks to identify baseline demographic and comorbid characteristics associated with survival outcomes and to evaluate the role of modifiable CVD risk factors in predicting all-cause mortality, or VTE.
Methods: We used the National Inpatient Sample (NIS) to extract data for all API patients aged >= 65 years hospitalized with CRC from 2016 to 2020 using ICD-10 CM codes. Prevalence and trends in VTE and in-hospital mortality were assessed using a linear by linear association test. Baseline demographics and comorbidities were compared between those who survived vs. those who had in-hospital mortality. Multivariable logistic regression was performed to evaluate the role of modifiable cardiovascular disease risk factors in predicting all-cause mortality, or VTE in this understudied population adjusting for potential confounders.
Results: Among 21,565 CRC-related hospitalizations in the elderly API during the study period, 1210 (5.6%) died during hospitalization. From 2016 to 2020, the prevalence of VTE increased significantly (0.9% to 2.6%, ptrend < 0.001). Patients who died were slightly older (median age 77 vs. 74 years), with higher proportions of males (56.2% vs. 54.2%). Medicare was the predominant payer type for both groups; however, income distribution showed patients who died came from the lowest income quartile compared to survivors (19.1% vs. 13.2%). Complicated hypertension (27.3% vs. 20.4%) and a prior history of cancer (87.6% vs. 66.7%) were more prevalent in patients who died, whereas hyperlipidemia was more common among survivors (45.7% vs. 26.9%). Obesity significantly increased the risk of VTE in elderly API patients with colorectal cancer (adjusted OR 4, 95% CI: 2.09–7.68, p < 0.001). Hyperlipidemia significantly reduced the risk of all-cause mortality (adjusted OR = 0.45, 95% CI: 0.33-0.61, p< 0.001).
Discussion: There was a rising trend in VTE among elderly API patients hospitalized with CRC. Obesity significantly increased the risk of VTE while hyperlipidemia decreased the risk of all-cause mortality. Understanding these trends is crucial for developing targeted interventions to reduce VTE incidence and improve survival rates.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Azra Kothawala, MBBS1, Asees Lubana, 2, Anisha Chhabra, 2, Shreya Madan, 2, Rupak Desai, MBBS3. P0247 - Contemporary Nationwide Trends and Predictors of Venous Thromboembolism and Mortality in Elderly Asian American and Pacific Islander Patients Hospitalized With Colorectal Cancer: A Comprehensive Analysis (2016-2020), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Jawaharlal Nehru Medical College, Belgaum, Karnataka, India; 2Desert Mountain High School, Scottsdale, AZ; 3Outcomes Research, Atlanta, GA
Introduction: Venous thromboembolic events (VTE) and associated mortality are critical concerns in colorectal cancer (CRC) hospitalizations. The Asian American and Pacific Islander (API) elderly population is understudied in this context. This study assesses contemporary trends in VTE and mortality among elderly API patients hospitalized for CRC. It seeks to identify baseline demographic and comorbid characteristics associated with survival outcomes and to evaluate the role of modifiable CVD risk factors in predicting all-cause mortality, or VTE.
Methods: We used the National Inpatient Sample (NIS) to extract data for all API patients aged >= 65 years hospitalized with CRC from 2016 to 2020 using ICD-10 CM codes. Prevalence and trends in VTE and in-hospital mortality were assessed using a linear by linear association test. Baseline demographics and comorbidities were compared between those who survived vs. those who had in-hospital mortality. Multivariable logistic regression was performed to evaluate the role of modifiable cardiovascular disease risk factors in predicting all-cause mortality, or VTE in this understudied population adjusting for potential confounders.
Results: Among 21,565 CRC-related hospitalizations in the elderly API during the study period, 1210 (5.6%) died during hospitalization. From 2016 to 2020, the prevalence of VTE increased significantly (0.9% to 2.6%, ptrend < 0.001). Patients who died were slightly older (median age 77 vs. 74 years), with higher proportions of males (56.2% vs. 54.2%). Medicare was the predominant payer type for both groups; however, income distribution showed patients who died came from the lowest income quartile compared to survivors (19.1% vs. 13.2%). Complicated hypertension (27.3% vs. 20.4%) and a prior history of cancer (87.6% vs. 66.7%) were more prevalent in patients who died, whereas hyperlipidemia was more common among survivors (45.7% vs. 26.9%). Obesity significantly increased the risk of VTE in elderly API patients with colorectal cancer (adjusted OR 4, 95% CI: 2.09–7.68, p < 0.001). Hyperlipidemia significantly reduced the risk of all-cause mortality (adjusted OR = 0.45, 95% CI: 0.33-0.61, p< 0.001).
Discussion: There was a rising trend in VTE among elderly API patients hospitalized with CRC. Obesity significantly increased the risk of VTE while hyperlipidemia decreased the risk of all-cause mortality. Understanding these trends is crucial for developing targeted interventions to reduce VTE incidence and improve survival rates.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Azra Kothawala indicated no relevant financial relationships.
Asees Lubana indicated no relevant financial relationships.
Anisha Chhabra indicated no relevant financial relationships.
Shreya Madan indicated no relevant financial relationships.
Rupak Desai indicated no relevant financial relationships.
Azra Kothawala, MBBS1, Asees Lubana, 2, Anisha Chhabra, 2, Shreya Madan, 2, Rupak Desai, MBBS3. P0247 - Contemporary Nationwide Trends and Predictors of Venous Thromboembolism and Mortality in Elderly Asian American and Pacific Islander Patients Hospitalized With Colorectal Cancer: A Comprehensive Analysis (2016-2020), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
