Sunday Poster Session
Category: Colon
P0255 - A Case of Non-Neutropenic Enterocolitis in a Renal Transplant Patient
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Busara Songtanin, MD
Texas Tech University Health Sciences Center
Lubbock, TX
Presenting Author(s)
Busara Songtanin, MD, Nicole Welch, MD, Cristian Castillo-Rodriguez, MD, Brian Schroeder, MD, MBA
Texas Tech University Health Sciences Center, Lubbock, TX
Introduction: Neutropenic enterocolitis, also known as typhlitis, is a critical condition typically seen in neutropenic patients. However, we present a unique case of typhlitis in a non-neutropenic patient who was immunosuppressed, leading to a disease process similar to typhlitis.
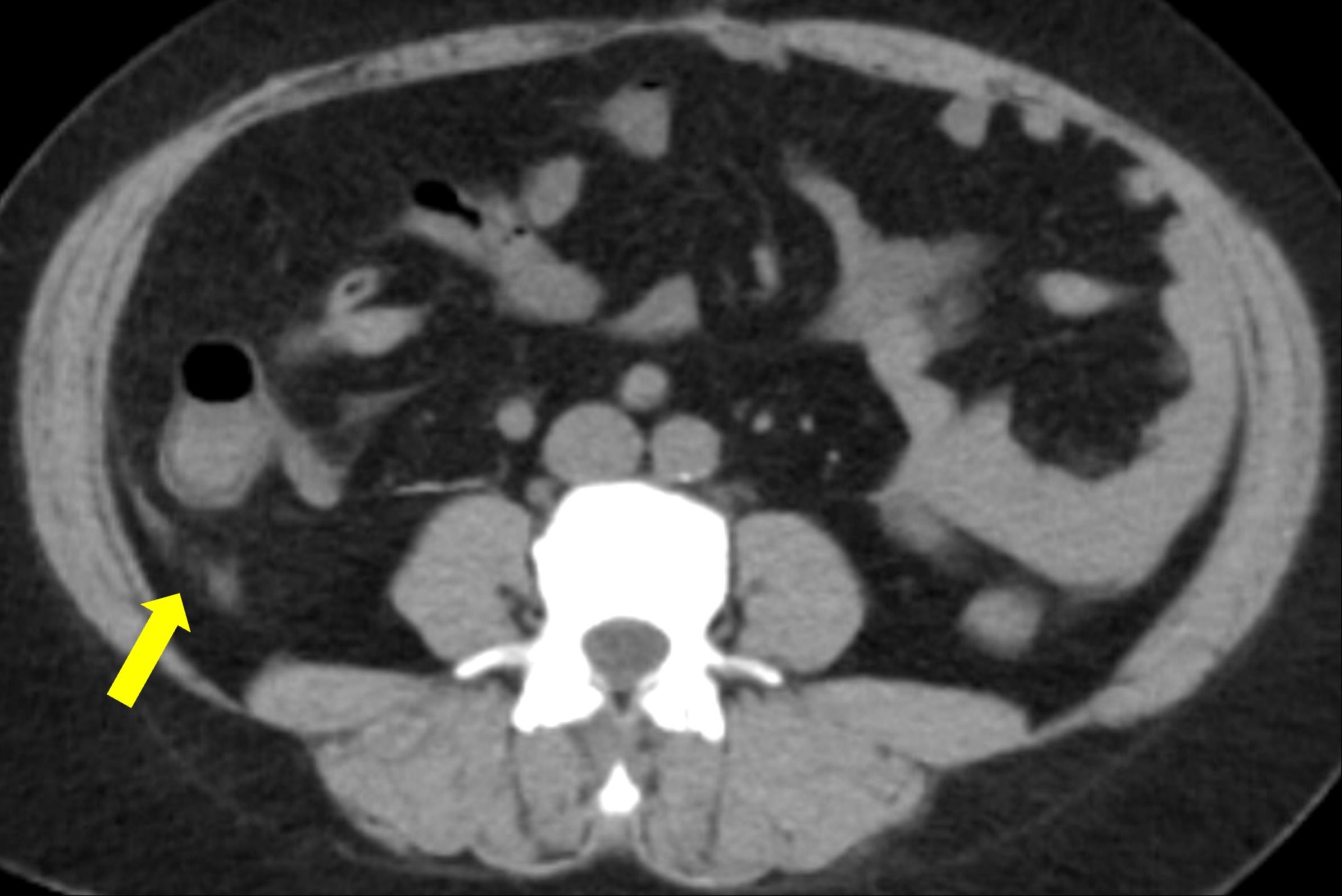
Case Description/Methods: A 50-year-old woman with a past medical history of end-stage renal disease secondary to autosomal dominant polycystic kidney disease and rheumatoid arthritis who underwent a kidney transplant six years ago presented to the hospital with abdominal pain and diarrhea for 3 days. The abdominal pain was associated with nausea, vomiting, and diarrhea. Her home medications include mycophenolate mofetil, tacrolimus, prednisone, and adalimumab. Vital signs showed a temperature 98.4 F, blood pressure 138/73 mmHg. Abdominal examination showed non-distended, soft, and tenderness at lower abdominal area. Laboratory showed Hgb 9.1 g/dL, WBC 11k/µL (reference range 4-11 k/µL) with neutrophil 82%, Cr 1.4 mg/dL, and liver functions were normal. Computed tomography of the abdomen and pelvis without contrast showed a small amount of free fluid adjacent to the cecum suggestive of typhlitis and normal appendix. Stool PCR (Shigella, Norovirus, Salmonella, Campylobacter, Yernisia, Vibrio), stool Giardia and Cryptosporidium, and stool Clostridium difficile were negative. Other workups, including BK and JC virus, were negative. The patient was given intravenous fluid and broad-spectrum antibiotics. She responded well to antibiotics and was discharged home in 7 days. Nephrology and infectious disease were consulted and decided to keep the patient on the same dose of immunosuppressive therapy and she continued to do well at the 2 weeks follow up.
Discussion: Neutropenic enterocolitis is a life-threatening condition that occurs primarily in neutropenic patients. The pathophysiology is unclear but thought to be related to the translocation of bacteria through the inflamed intestinal wall and impaired host defense to invasion by polymicrobial organisms. The diagnostic criteria are based on clinical manifestation, laboratory, and imaging.
While typhlitis is predominantly seen in neutropenic patients, our case highlights the importance of considering it in non-neutropenic, immunosuppressed individuals. The timely administration of broad-spectrum antibiotics and intravenous fluids, along with ruling out other causes of enterocolitis, are crucial in managing non-neutropenic typhlitis.
Disclosures:
Busara Songtanin, MD, Nicole Welch, MD, Cristian Castillo-Rodriguez, MD, Brian Schroeder, MD, MBA. P0255 - A Case of Non-Neutropenic Enterocolitis in a Renal Transplant Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Texas Tech University Health Sciences Center, Lubbock, TX
Introduction: Neutropenic enterocolitis, also known as typhlitis, is a critical condition typically seen in neutropenic patients. However, we present a unique case of typhlitis in a non-neutropenic patient who was immunosuppressed, leading to a disease process similar to typhlitis.
Case Description/Methods: A 50-year-old woman with a past medical history of end-stage renal disease secondary to autosomal dominant polycystic kidney disease and rheumatoid arthritis who underwent a kidney transplant six years ago presented to the hospital with abdominal pain and diarrhea for 3 days. The abdominal pain was associated with nausea, vomiting, and diarrhea. Her home medications include mycophenolate mofetil, tacrolimus, prednisone, and adalimumab. Vital signs showed a temperature 98.4 F, blood pressure 138/73 mmHg. Abdominal examination showed non-distended, soft, and tenderness at lower abdominal area. Laboratory showed Hgb 9.1 g/dL, WBC 11k/µL (reference range 4-11 k/µL) with neutrophil 82%, Cr 1.4 mg/dL, and liver functions were normal. Computed tomography of the abdomen and pelvis without contrast showed a small amount of free fluid adjacent to the cecum suggestive of typhlitis and normal appendix. Stool PCR (Shigella, Norovirus, Salmonella, Campylobacter, Yernisia, Vibrio), stool Giardia and Cryptosporidium, and stool Clostridium difficile were negative. Other workups, including BK and JC virus, were negative. The patient was given intravenous fluid and broad-spectrum antibiotics. She responded well to antibiotics and was discharged home in 7 days. Nephrology and infectious disease were consulted and decided to keep the patient on the same dose of immunosuppressive therapy and she continued to do well at the 2 weeks follow up.
Discussion: Neutropenic enterocolitis is a life-threatening condition that occurs primarily in neutropenic patients. The pathophysiology is unclear but thought to be related to the translocation of bacteria through the inflamed intestinal wall and impaired host defense to invasion by polymicrobial organisms. The diagnostic criteria are based on clinical manifestation, laboratory, and imaging.
While typhlitis is predominantly seen in neutropenic patients, our case highlights the importance of considering it in non-neutropenic, immunosuppressed individuals. The timely administration of broad-spectrum antibiotics and intravenous fluids, along with ruling out other causes of enterocolitis, are crucial in managing non-neutropenic typhlitis.
Figure: CT abdomen and pelvis without contrast showed a small amount of free fluid near the cecum (yellow arrow).
Disclosures:
Busara Songtanin indicated no relevant financial relationships.
Nicole Welch indicated no relevant financial relationships.
Cristian Castillo-Rodriguez indicated no relevant financial relationships.
Brian Schroeder indicated no relevant financial relationships.
Busara Songtanin, MD, Nicole Welch, MD, Cristian Castillo-Rodriguez, MD, Brian Schroeder, MD, MBA. P0255 - A Case of Non-Neutropenic Enterocolitis in a Renal Transplant Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
