Sunday Poster Session
Category: Colon
P0279 - A Rare Case of Primary Gastrointestinal Mantle Cell Lymphoma Hiding in Plain Sight as Colon Polyps
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Suhaib Alhaj Ali, MD
Henry Ford Hospital
Detroit, MI
Presenting Author(s)
Suhib Alhaj Ali, MD1, Polo Kostecki, DO1, Muhammad Zarrar Khan, MD2, Amit Bhan, MD1
1Henry Ford Hospital, Detroit, MI; 2Henry Ford Hospital, Royal Oak, MI
Introduction: Mantle cell lymphoma (MCL) is an aggressive subtype of B cell non-Hodgkin lymphoma that constitutes only a small fraction (0.4%) of all primary gastrointestinal lymphomas. Patients with MCL have a high relapse rate and poor prognosis.
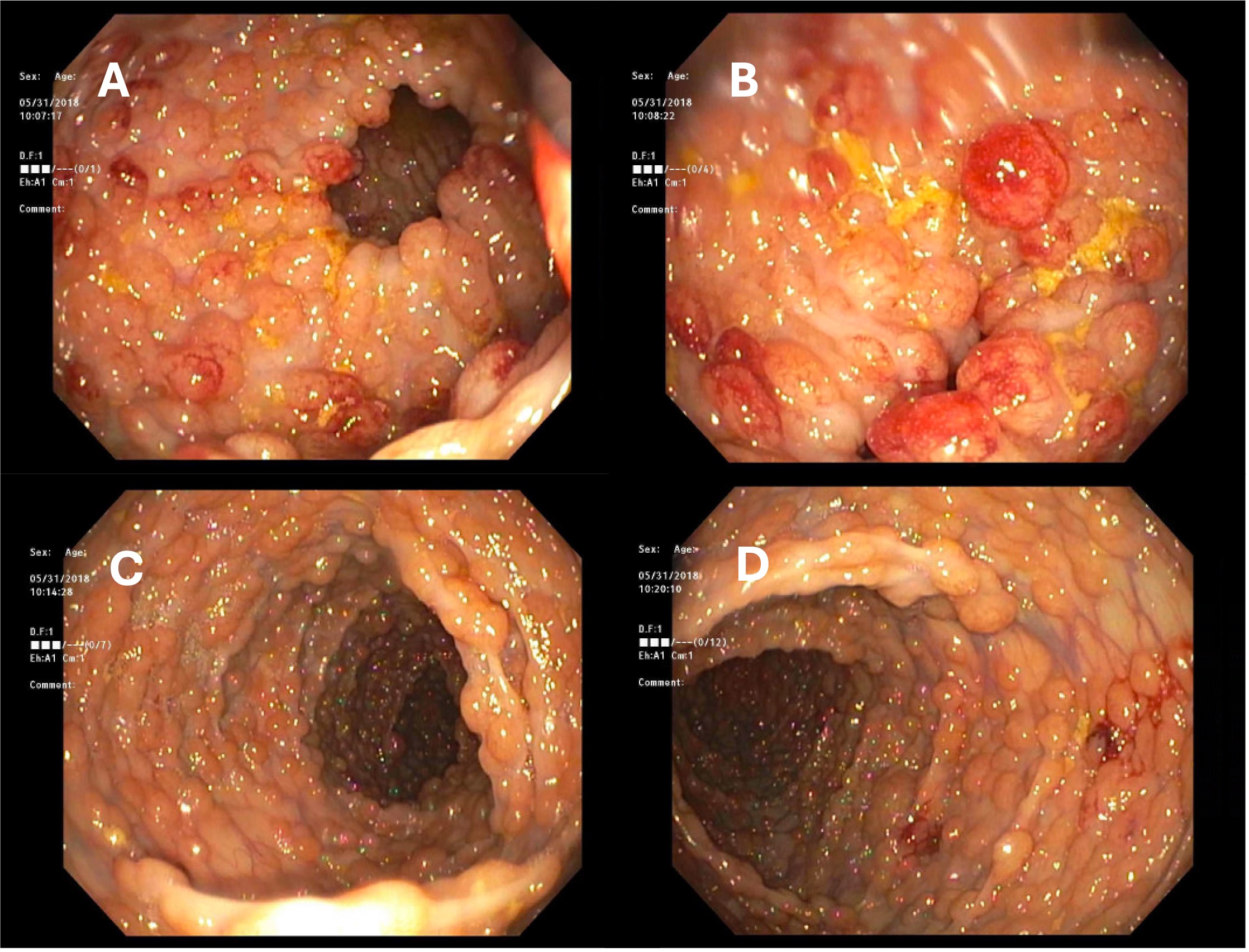
Case Description/Methods: A 71-year-old man presented with 6 months of non-specific symptoms including abdominal discomfort, altered bowel habits, and weight loss. Although he had a normal colonoscopy 4 years prior, a repeat endoscopic examination revealed significant lymphomatous polyposis, with hundreds of non-bleeding polyps localized from the rectum to the distal ascending colon. Histopathological assessment of the polyps revealed a lymphoid infiltrate consistent with MCL. Cytogenetic analysis of bone marrow aspirate along with imaging revealing extensive mesenteric and retroperitoneal adenopathy and a mildly enlarged spleen confirmed the MCL diagnosis. The patient underwent 6 cycles of bendamustine and rituximab followed by maintenance rituximab therapy every 2 months. Throughout and after treatment, serial imaging showed markedly reduced adenopathy, and colonoscopy performed 2 months post-treatment (prior to maintenance therapy) demonstrated completely normal colon without evidence of any residual polyps. One month after completing initial chemotherapy, an incidental complex renal lesion was diagnosed as clear-cell renal cell carcinoma (World Health Organization / International Society of Urologic Pathologists grade 1, 4 cm, limited to the kidney), and the patient underwent successful partial nephrectomy after completion of chemotherapy.
Discussion: Our case underscores the imperativeness of thorough endoscopic evaluation in patients with non-specific gastrointestinal symptoms to ensure early detection and effective management of rare colonic cancers. This is particularly important with classic “red-flag” symptoms and features suggesting malignancy and despite normal recent colonoscopies (as in our patient who had a normal colonoscopy 4 years prior). The case further highlights how quickly the rare condition of gastrointestinal MCL can arise, necessitating swift immunohistochemical, imaging, and cytogenetic analysis to identify this aggressive condition. Even with a delayed presentation and diagnosis, diligent and timely treatment can still result in significant disease remission. The co-occurrence of gastrointestinal MCL with renal cell carcinoma introduces additional complexity to the case and suggests a potential association warranting further study.
Disclosures:
Suhib Alhaj Ali, MD1, Polo Kostecki, DO1, Muhammad Zarrar Khan, MD2, Amit Bhan, MD1. P0279 - A Rare Case of Primary Gastrointestinal Mantle Cell Lymphoma Hiding in Plain Sight as Colon Polyps, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Henry Ford Hospital, Detroit, MI; 2Henry Ford Hospital, Royal Oak, MI
Introduction: Mantle cell lymphoma (MCL) is an aggressive subtype of B cell non-Hodgkin lymphoma that constitutes only a small fraction (0.4%) of all primary gastrointestinal lymphomas. Patients with MCL have a high relapse rate and poor prognosis.
Case Description/Methods: A 71-year-old man presented with 6 months of non-specific symptoms including abdominal discomfort, altered bowel habits, and weight loss. Although he had a normal colonoscopy 4 years prior, a repeat endoscopic examination revealed significant lymphomatous polyposis, with hundreds of non-bleeding polyps localized from the rectum to the distal ascending colon. Histopathological assessment of the polyps revealed a lymphoid infiltrate consistent with MCL. Cytogenetic analysis of bone marrow aspirate along with imaging revealing extensive mesenteric and retroperitoneal adenopathy and a mildly enlarged spleen confirmed the MCL diagnosis. The patient underwent 6 cycles of bendamustine and rituximab followed by maintenance rituximab therapy every 2 months. Throughout and after treatment, serial imaging showed markedly reduced adenopathy, and colonoscopy performed 2 months post-treatment (prior to maintenance therapy) demonstrated completely normal colon without evidence of any residual polyps. One month after completing initial chemotherapy, an incidental complex renal lesion was diagnosed as clear-cell renal cell carcinoma (World Health Organization / International Society of Urologic Pathologists grade 1, 4 cm, limited to the kidney), and the patient underwent successful partial nephrectomy after completion of chemotherapy.
Discussion: Our case underscores the imperativeness of thorough endoscopic evaluation in patients with non-specific gastrointestinal symptoms to ensure early detection and effective management of rare colonic cancers. This is particularly important with classic “red-flag” symptoms and features suggesting malignancy and despite normal recent colonoscopies (as in our patient who had a normal colonoscopy 4 years prior). The case further highlights how quickly the rare condition of gastrointestinal MCL can arise, necessitating swift immunohistochemical, imaging, and cytogenetic analysis to identify this aggressive condition. Even with a delayed presentation and diagnosis, diligent and timely treatment can still result in significant disease remission. The co-occurrence of gastrointestinal MCL with renal cell carcinoma introduces additional complexity to the case and suggests a potential association warranting further study.
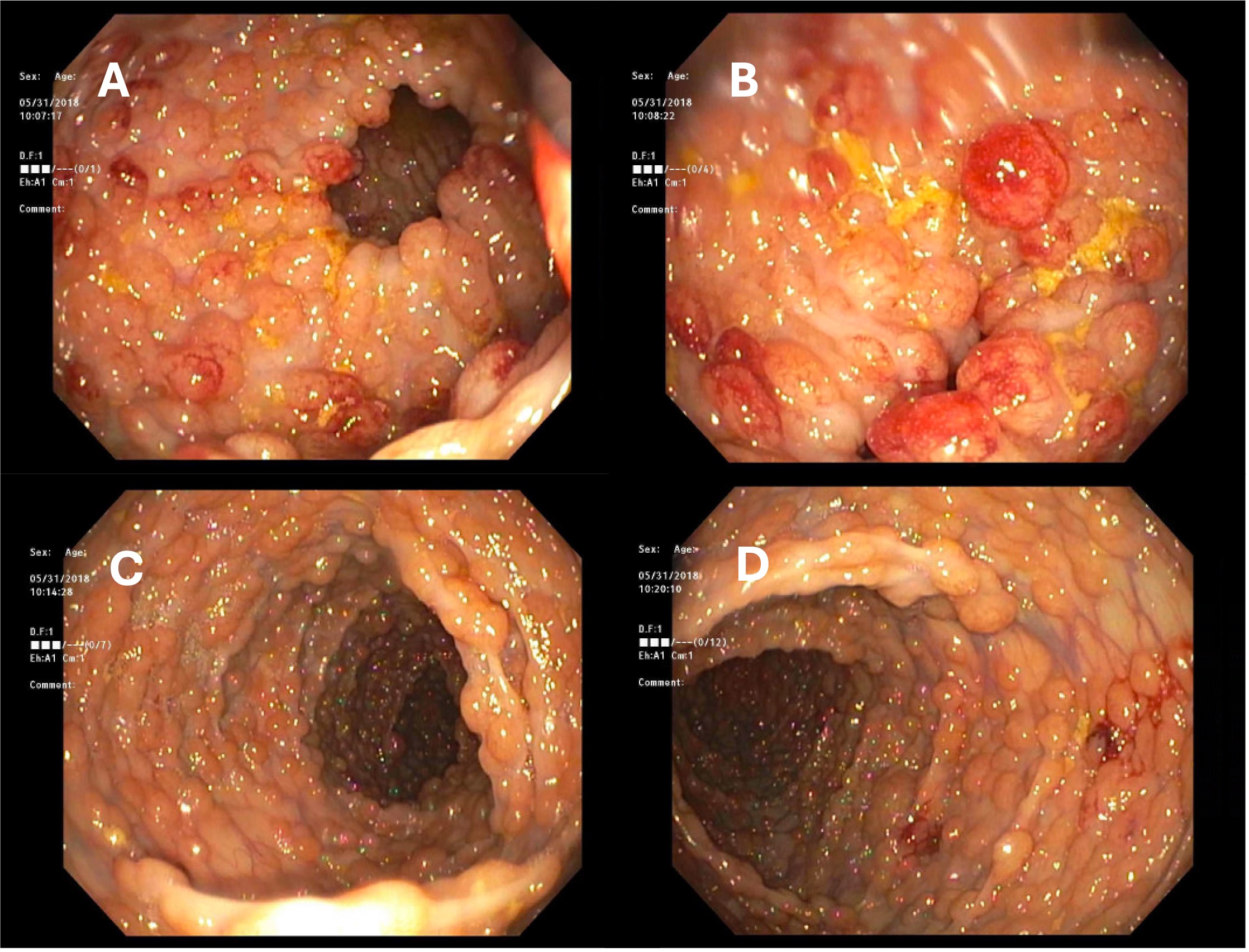
Figure: Fig. 1. Many 5 to 25 mm, non-bleeding polyps throughout the colon, including the sigmoid (A), descending (B), transverse (C), and ascending (D) colon.
Disclosures:
Suhib Alhaj Ali indicated no relevant financial relationships.
Polo Kostecki indicated no relevant financial relationships.
Muhammad Zarrar Khan indicated no relevant financial relationships.
Amit Bhan indicated no relevant financial relationships.
Suhib Alhaj Ali, MD1, Polo Kostecki, DO1, Muhammad Zarrar Khan, MD2, Amit Bhan, MD1. P0279 - A Rare Case of Primary Gastrointestinal Mantle Cell Lymphoma Hiding in Plain Sight as Colon Polyps, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
