Sunday Poster Session
Category: Colon
P0283 - The Battle Against CMV in Transplant Patients: A Case of Antiviral Resistance
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Aayushi J. Rajani, MBBS
Government Medical College and Hospital
Vadodara, Gujarat, India
Presenting Author(s)
Aayushi J. Rajani, MBBS1, Mipasha Patel, MBBS2, Juhi Amin, MBBS, MS1, Rubela Ray, MBBS3, Nritya Trivedi, MBBS4, Darshan Raval, MBBS, MD5
1Government Medical College and Hospital, Vadodara, Gujarat, India; 2Government Medical College and Hospital, New Jersey, NJ; 3Government Medical College and Hospital, Bankura, West Bengal, India; 4Government Medical College and Hospital, Bharuch, Gujarat, India; 5Western Reserve Health Education, Warren, OH
Introduction: Cytomegalovirus (CMV) infection poses a significant challenge in transplant patients due to limited treatment options and potential antiviral resistance. Management is difficult due to poor drug sensitivity, with only Valganciclovir, Maribavir, and Letermovir used in current practice, necessitating careful approaches to avoid drug resistance.
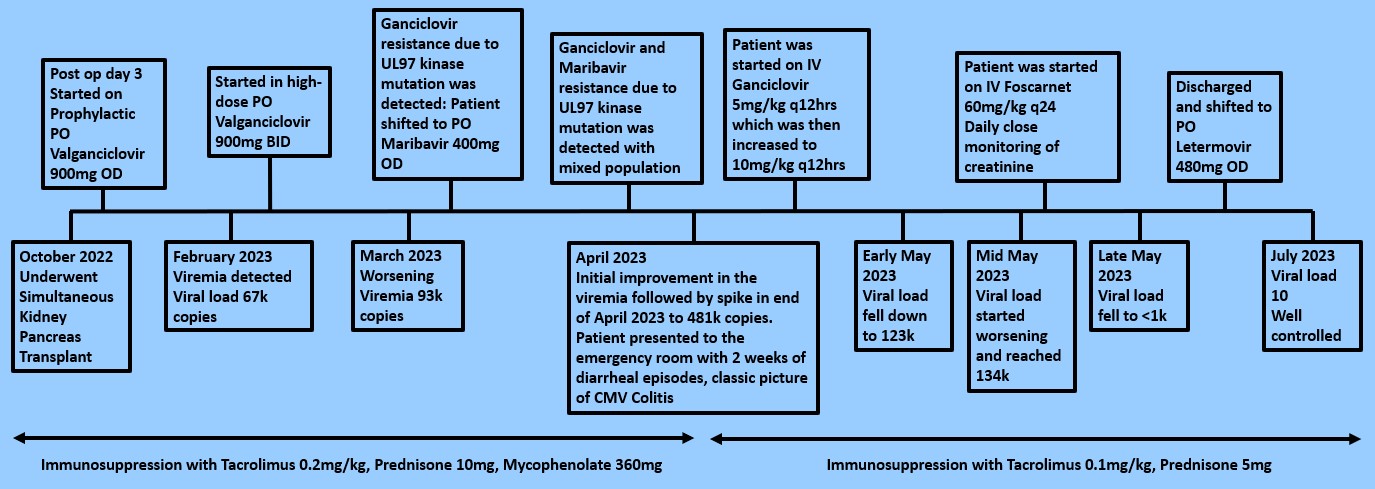
Case Description/Methods: A 51-year-old female with type 2 DM, HTN, hyperlipidemia, ESRD, and VHL syndrome underwent simultaneous kidney-pancreas transplantation. Postoperatively, she was started on Tacrolimus, Prednisone, Mycophenolate, Valganciclovir, and Sulfamethoxazole-Trimethoprim. Despite prophylactic PO Valganciclovir 900 mg daily, she developed a high viral load of 67,000 IU/mL. Increasing the dose to twice daily did not help, and with Ganciclovir-resistant mutations, her viral load rose even more. Treatment was switched to PO Maribavir, which initially caused a significant reduction in the viral load. However, mutations in the UL97 kinase gene led to resistance to both Ganciclovir and Maribavir.
In late April, she presented with persistent watery diarrhea, chills, tremors, severe fatigue, and an elevated viral load of 472,000 IU/mL. A colonoscopy revealed widespread erythematous and ulcerated mucosa throughout the colon, diagnostic of CMV colitis. High-dose IV Ganciclovir initially reduced the viral load by early May but it started rising soon after, indicating a mixed population of CMV strains. Initial drug administration would target the wild-type strain, but the resistant strains would keep growing. IV Foscarnet, to which she had no documented resistance, was started, reducing the viral load below 1,000 IU/mL by the end of May. She was then transitioned to PO Letermovir.
Discussion: Treatment includes appropriate antiviral use, CMV PCR monitoring, resistance screening, and managing side effects. Treating CMV colitis is challenging due to agent toxicity and transplant-related complications. There are only three oral drugs: Valganciclovir, Maribavir, and Letermovir, and limited IV options: Ganciclovir, Foscarnet, and Cidofovir. This case adds to the limited literature on resistant CMV colitis, emphasizing the need for continuous viral load monitoring and flexible therapy adjustments. An initial positive response doesn't negate the need for ongoing observation, as improvement might precede a sudden viral load increase. Further research and comprehensive guidelines are necessary to advance CMV management in solid organ transplant patients.
Disclosures:
Aayushi J. Rajani, MBBS1, Mipasha Patel, MBBS2, Juhi Amin, MBBS, MS1, Rubela Ray, MBBS3, Nritya Trivedi, MBBS4, Darshan Raval, MBBS, MD5. P0283 - The Battle Against CMV in Transplant Patients: A Case of Antiviral Resistance, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Government Medical College and Hospital, Vadodara, Gujarat, India; 2Government Medical College and Hospital, New Jersey, NJ; 3Government Medical College and Hospital, Bankura, West Bengal, India; 4Government Medical College and Hospital, Bharuch, Gujarat, India; 5Western Reserve Health Education, Warren, OH
Introduction: Cytomegalovirus (CMV) infection poses a significant challenge in transplant patients due to limited treatment options and potential antiviral resistance. Management is difficult due to poor drug sensitivity, with only Valganciclovir, Maribavir, and Letermovir used in current practice, necessitating careful approaches to avoid drug resistance.
Case Description/Methods: A 51-year-old female with type 2 DM, HTN, hyperlipidemia, ESRD, and VHL syndrome underwent simultaneous kidney-pancreas transplantation. Postoperatively, she was started on Tacrolimus, Prednisone, Mycophenolate, Valganciclovir, and Sulfamethoxazole-Trimethoprim. Despite prophylactic PO Valganciclovir 900 mg daily, she developed a high viral load of 67,000 IU/mL. Increasing the dose to twice daily did not help, and with Ganciclovir-resistant mutations, her viral load rose even more. Treatment was switched to PO Maribavir, which initially caused a significant reduction in the viral load. However, mutations in the UL97 kinase gene led to resistance to both Ganciclovir and Maribavir.
In late April, she presented with persistent watery diarrhea, chills, tremors, severe fatigue, and an elevated viral load of 472,000 IU/mL. A colonoscopy revealed widespread erythematous and ulcerated mucosa throughout the colon, diagnostic of CMV colitis. High-dose IV Ganciclovir initially reduced the viral load by early May but it started rising soon after, indicating a mixed population of CMV strains. Initial drug administration would target the wild-type strain, but the resistant strains would keep growing. IV Foscarnet, to which she had no documented resistance, was started, reducing the viral load below 1,000 IU/mL by the end of May. She was then transitioned to PO Letermovir.
Discussion: Treatment includes appropriate antiviral use, CMV PCR monitoring, resistance screening, and managing side effects. Treating CMV colitis is challenging due to agent toxicity and transplant-related complications. There are only three oral drugs: Valganciclovir, Maribavir, and Letermovir, and limited IV options: Ganciclovir, Foscarnet, and Cidofovir. This case adds to the limited literature on resistant CMV colitis, emphasizing the need for continuous viral load monitoring and flexible therapy adjustments. An initial positive response doesn't negate the need for ongoing observation, as improvement might precede a sudden viral load increase. Further research and comprehensive guidelines are necessary to advance CMV management in solid organ transplant patients.
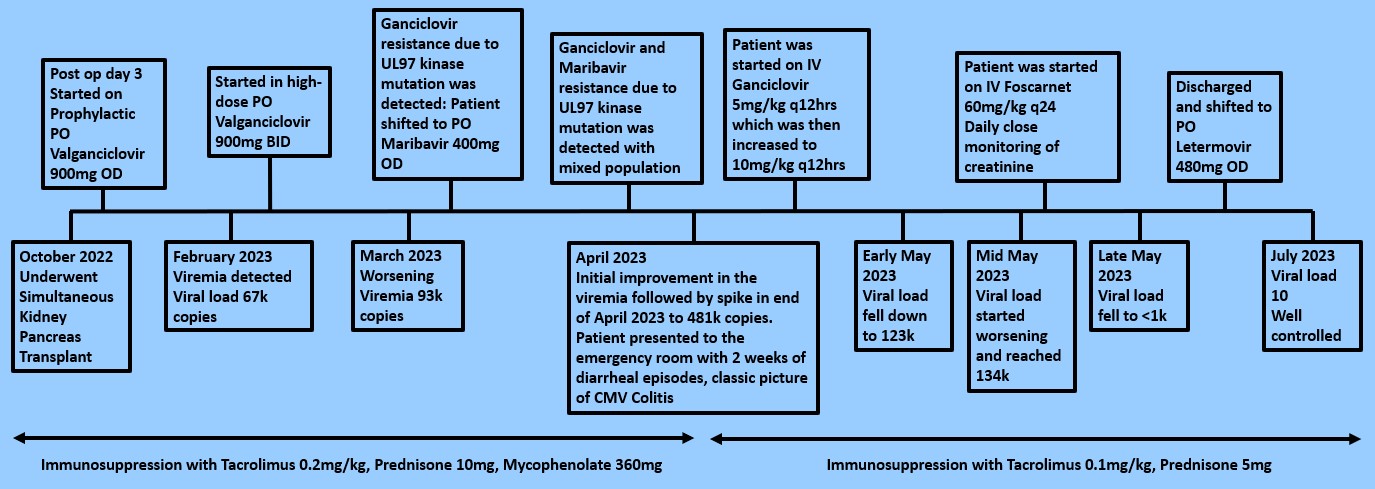
Figure: Timeline covering the progression of CMV colitis, the development of resistance and various management strategies to symptom resolution spanning over 9 months
Disclosures:
Aayushi Rajani indicated no relevant financial relationships.
Mipasha Patel indicated no relevant financial relationships.
Juhi Amin indicated no relevant financial relationships.
Rubela Ray indicated no relevant financial relationships.
Nritya Trivedi indicated no relevant financial relationships.
Darshan Raval indicated no relevant financial relationships.
Aayushi J. Rajani, MBBS1, Mipasha Patel, MBBS2, Juhi Amin, MBBS, MS1, Rubela Ray, MBBS3, Nritya Trivedi, MBBS4, Darshan Raval, MBBS, MD5. P0283 - The Battle Against CMV in Transplant Patients: A Case of Antiviral Resistance, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
