Sunday Poster Session
Category: Colon
P0284 - Cyclospora cayetanensis or Clostridium difficile: Who Caused the Diarrhea?
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Aayushi J. Rajani, MBBS
Government Medical College and Hospital
Vadodara, Gujarat, India
Presenting Author(s)
Aayushi J. Rajani, MBBS1, Shashwat Mallik, MBBS1, Shahin Khan, MBBS1, Juhi Amin, MBBS, MS1, Mipasha Patel, MBBS2, Nritya Trivedi, MBBS3, Velagapudi Keerthi. Bala, MBBS4, Vaishnavi M. Rathod, MBBS, MD1, Darshan Raval, MBBS, MD5
1Government Medical College and Hospital, Vadodara, Gujarat, India; 2Government Medical College and Hospital, New Jersey, NJ; 3Government Medical College and Hospital, Bharuch, Gujarat, India; 4Dr. Pinnamaneni Siddhartha Institute of Medical Sciences and Research Foundation, Gannavaram, Andhra Pradesh, India; 5Western Reserve Health Education, Warren, OH
Introduction: Cyclospora cayetanensis, a parasite causing human enteritis, has been rarely reported from healthcare laboratories, despite its universal presence. Most cases of cyclosporiasis in developed nations are associated with a history of international travel or the consumption of imported fruits and vegetables. While it is usually responsible for self-limiting diarrhea in immunocompetent individuals, we present a case where the patient suffered from severe, unrelenting diarrhea despite having no obvious immune defects. Clostridium difficile (C. difficile) is an opportunistic bacterial pathogen that is another cause of intestinal diseases in humans, ranging from antibiotic-induced diarrhea to pseudomembranous colitis. Our case describes a diagnostic dilemma to ascertain what the causative agent for the patient’s diarrhea was.
Case Description/Methods: A 60-year-old immunocompetent woman with no history of international travel or consumption of outside food or water presented with a bout of diarrhea. A week after testing positive only for cyclospora, the patient returned with a high-grade fever. She subsequently tested positive for Clostridium difficile as well, and her diarrhea showed no signs of improvement. This posed a dilemma for the clinicians as the patient was suffering from diarrhea even when she had tested negative for Clostridium difficile, but she recovered only when fidaxomicin was prescribed. To add to the perplexity, Cyclospora remained positive in her stool even after the completion of the prescribed treatment.
Discussion: Several hypotheses have been derived from this unusual case, and the most probable one seems to be a case of co-infection; however, such a co-infection has never been reported in the literature. Another possibility is chronic gut colonization by Cyclospora without infection, which may have altered the gut microbiota and decreased mucosal immunity, leading to the patient developing C. difficile colitis via a mechanism similar to that seen in antibiotic-induced diarrhea. This case report serves as a unique opportunity to explore the possible mechanisms, if any, regarding how Cyclospora infection or colonization may predispose individuals to C. difficile infection.
Disclosures:
Aayushi J. Rajani, MBBS1, Shashwat Mallik, MBBS1, Shahin Khan, MBBS1, Juhi Amin, MBBS, MS1, Mipasha Patel, MBBS2, Nritya Trivedi, MBBS3, Velagapudi Keerthi. Bala, MBBS4, Vaishnavi M. Rathod, MBBS, MD1, Darshan Raval, MBBS, MD5. P0284 - <i>Cyclospora cayetanensis</i> or <i>Clostridium difficile</i>: Who Caused the Diarrhea?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Government Medical College and Hospital, Vadodara, Gujarat, India; 2Government Medical College and Hospital, New Jersey, NJ; 3Government Medical College and Hospital, Bharuch, Gujarat, India; 4Dr. Pinnamaneni Siddhartha Institute of Medical Sciences and Research Foundation, Gannavaram, Andhra Pradesh, India; 5Western Reserve Health Education, Warren, OH
Introduction: Cyclospora cayetanensis, a parasite causing human enteritis, has been rarely reported from healthcare laboratories, despite its universal presence. Most cases of cyclosporiasis in developed nations are associated with a history of international travel or the consumption of imported fruits and vegetables. While it is usually responsible for self-limiting diarrhea in immunocompetent individuals, we present a case where the patient suffered from severe, unrelenting diarrhea despite having no obvious immune defects. Clostridium difficile (C. difficile) is an opportunistic bacterial pathogen that is another cause of intestinal diseases in humans, ranging from antibiotic-induced diarrhea to pseudomembranous colitis. Our case describes a diagnostic dilemma to ascertain what the causative agent for the patient’s diarrhea was.
Case Description/Methods: A 60-year-old immunocompetent woman with no history of international travel or consumption of outside food or water presented with a bout of diarrhea. A week after testing positive only for cyclospora, the patient returned with a high-grade fever. She subsequently tested positive for Clostridium difficile as well, and her diarrhea showed no signs of improvement. This posed a dilemma for the clinicians as the patient was suffering from diarrhea even when she had tested negative for Clostridium difficile, but she recovered only when fidaxomicin was prescribed. To add to the perplexity, Cyclospora remained positive in her stool even after the completion of the prescribed treatment.
Discussion: Several hypotheses have been derived from this unusual case, and the most probable one seems to be a case of co-infection; however, such a co-infection has never been reported in the literature. Another possibility is chronic gut colonization by Cyclospora without infection, which may have altered the gut microbiota and decreased mucosal immunity, leading to the patient developing C. difficile colitis via a mechanism similar to that seen in antibiotic-induced diarrhea. This case report serves as a unique opportunity to explore the possible mechanisms, if any, regarding how Cyclospora infection or colonization may predispose individuals to C. difficile infection.
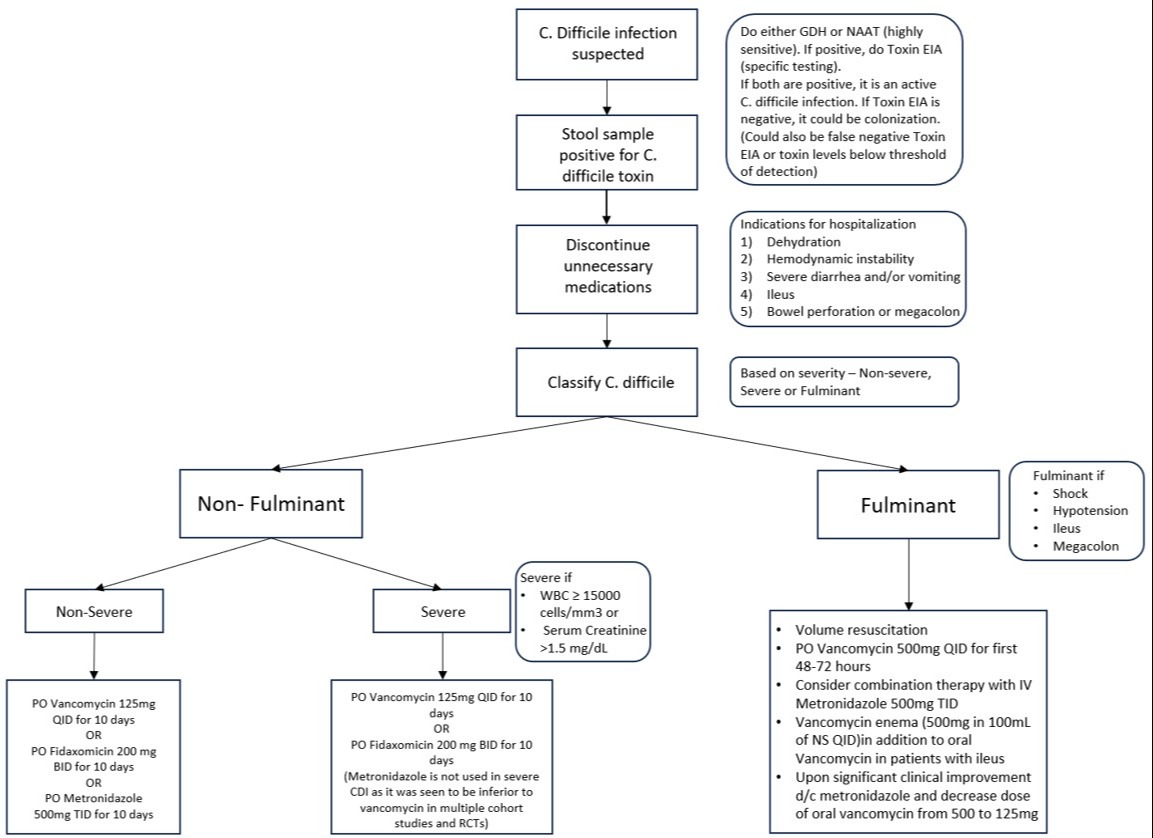
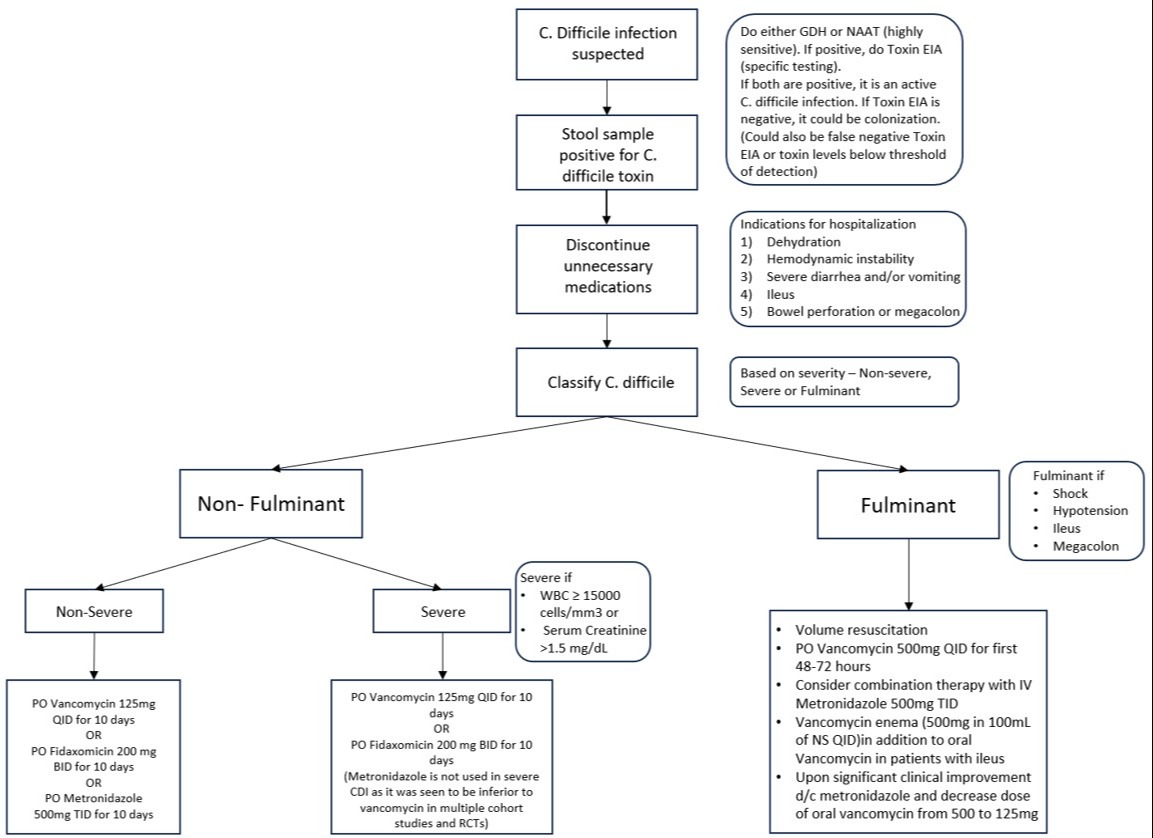
Figure: Suggested guidelines for the management of C. difficile infection
Disclosures:
Aayushi Rajani indicated no relevant financial relationships.
Shashwat Mallik indicated no relevant financial relationships.
Shahin Khan indicated no relevant financial relationships.
Juhi Amin indicated no relevant financial relationships.
Mipasha Patel indicated no relevant financial relationships.
Nritya Trivedi indicated no relevant financial relationships.
Velagapudi Bala indicated no relevant financial relationships.
Vaishnavi Rathod indicated no relevant financial relationships.
Darshan Raval indicated no relevant financial relationships.
Aayushi J. Rajani, MBBS1, Shashwat Mallik, MBBS1, Shahin Khan, MBBS1, Juhi Amin, MBBS, MS1, Mipasha Patel, MBBS2, Nritya Trivedi, MBBS3, Velagapudi Keerthi. Bala, MBBS4, Vaishnavi M. Rathod, MBBS, MD1, Darshan Raval, MBBS, MD5. P0284 - <i>Cyclospora cayetanensis</i> or <i>Clostridium difficile</i>: Who Caused the Diarrhea?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
