Sunday Poster Session
Category: Colon
P0290 - Diagnostic Challenges and Effective Treatment of Gastrointestinal TB: Insights From a Clinical Case
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E

- RR
Rajmohan Rammohan, MD
Nassau University Medical Center
East Meadow, NY
Presenting Author(s)
Raj Mohan Ram Mohan, MD, Leeza Pannikodu, MD, Sai Reshma Magam, MD, Sai Greeshma Magam, MD, Melvin Joy, MD, Dilman Natt, MD, Abhishek Tadikonda, MD, Winghang Lau, MD, Jiten Desai, MD, Paul Mustacchia, MD, MBA
Nassau University Medical Center, East Meadow, NY
Introduction: Gastrointestinal tuberculosis (TB) is rare, accounting for 1% to 3% of all TB cases worldwide. The ileocecal region is the most affected site; gastrointestinal TB can involve any part of the gastrointestinal tract. The combination of clinical examination, conventional examination, and the latest molecular-based examination is the best choice for diagnosing intestinal tuberculosis. High clinical suspicion, early initiation of anti-tuberculous therapy, and involvement of an interprofessional team are necessary for reducing morbidity and mortality. Surgery is only required in cases that develop complications such as strictures or obstruction, and in those cases that are unresponsive to medical therapy.
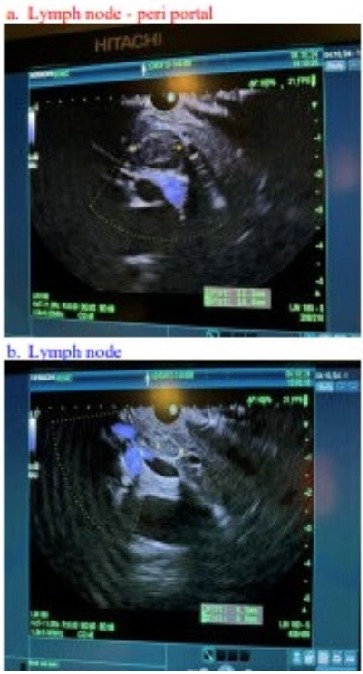
Case Description/Methods: A 21-year-old Haitian male presented to the ED with a cough, vomiting, and diarrhea for one week. His cough was associated with white sputum with a small tinge of blood in some episodes. His labs were significant for anemia. Chest x-ray revealed loculated pleural effusion of the right upper lobe with bilateral reticulonodular opacities. Sputum AFB x3 was positive indicating likely active pulmonary TB. CT and MRI showed involvement of the pancreatic head and hepatic hilum. Endoscopic ultrasound revealed a small peri-portal lymph node. The patient was subsequently treated with RIPE therapy for 9 months. MRI of the abdomen after treatment showed a decrease in necrotic appearing porto-caval adenopathy and MRCP revealed a mildly lobulated lesion within the region of the porta hepatis/pancreaticoduodenal groove that had decreased in size measuring approximately 3.5cm x 1.7cm, previously measuring 4.9cm x 2.6cm.
Discussion: Intestinal TB can be misdiagnosed as IBD with the administration of steroids, potentially worsening infection. The disease may mimic other conditions such as lymphoma, amebiasis, and adenocarcinoma. In a case series involving 49 patients with abdominal tuberculosis, Sinan et al. stratified identified the main symptoms and imaging findings. Fever(75%), abdominal pain(65%), and weight loss(36%) had a higher prevalence than other signs and symptoms. Peritonitis(38%) was the main tomographic finding, followed by lymph node disease(23%), involvement of the gastrointestinal tract(19%) and solid organs(10%). A diffuse pattern of lymph node commitment was most observed(48%). In the gastrointestinal tract, the terminal ileum and the ileocecal region were most remarkably affected(50%). Among other organs, the liver and spleen presented greater involvement(70%).
Disclosures:
Raj Mohan Ram Mohan, MD, Leeza Pannikodu, MD, Sai Reshma Magam, MD, Sai Greeshma Magam, MD, Melvin Joy, MD, Dilman Natt, MD, Abhishek Tadikonda, MD, Winghang Lau, MD, Jiten Desai, MD, Paul Mustacchia, MD, MBA. P0290 - Diagnostic Challenges and Effective Treatment of Gastrointestinal TB: Insights From a Clinical Case, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Nassau University Medical Center, East Meadow, NY
Introduction: Gastrointestinal tuberculosis (TB) is rare, accounting for 1% to 3% of all TB cases worldwide. The ileocecal region is the most affected site; gastrointestinal TB can involve any part of the gastrointestinal tract. The combination of clinical examination, conventional examination, and the latest molecular-based examination is the best choice for diagnosing intestinal tuberculosis. High clinical suspicion, early initiation of anti-tuberculous therapy, and involvement of an interprofessional team are necessary for reducing morbidity and mortality. Surgery is only required in cases that develop complications such as strictures or obstruction, and in those cases that are unresponsive to medical therapy.
Case Description/Methods: A 21-year-old Haitian male presented to the ED with a cough, vomiting, and diarrhea for one week. His cough was associated with white sputum with a small tinge of blood in some episodes. His labs were significant for anemia. Chest x-ray revealed loculated pleural effusion of the right upper lobe with bilateral reticulonodular opacities. Sputum AFB x3 was positive indicating likely active pulmonary TB. CT and MRI showed involvement of the pancreatic head and hepatic hilum. Endoscopic ultrasound revealed a small peri-portal lymph node. The patient was subsequently treated with RIPE therapy for 9 months. MRI of the abdomen after treatment showed a decrease in necrotic appearing porto-caval adenopathy and MRCP revealed a mildly lobulated lesion within the region of the porta hepatis/pancreaticoduodenal groove that had decreased in size measuring approximately 3.5cm x 1.7cm, previously measuring 4.9cm x 2.6cm.
Discussion: Intestinal TB can be misdiagnosed as IBD with the administration of steroids, potentially worsening infection. The disease may mimic other conditions such as lymphoma, amebiasis, and adenocarcinoma. In a case series involving 49 patients with abdominal tuberculosis, Sinan et al. stratified identified the main symptoms and imaging findings. Fever(75%), abdominal pain(65%), and weight loss(36%) had a higher prevalence than other signs and symptoms. Peritonitis(38%) was the main tomographic finding, followed by lymph node disease(23%), involvement of the gastrointestinal tract(19%) and solid organs(10%). A diffuse pattern of lymph node commitment was most observed(48%). In the gastrointestinal tract, the terminal ileum and the ileocecal region were most remarkably affected(50%). Among other organs, the liver and spleen presented greater involvement(70%).
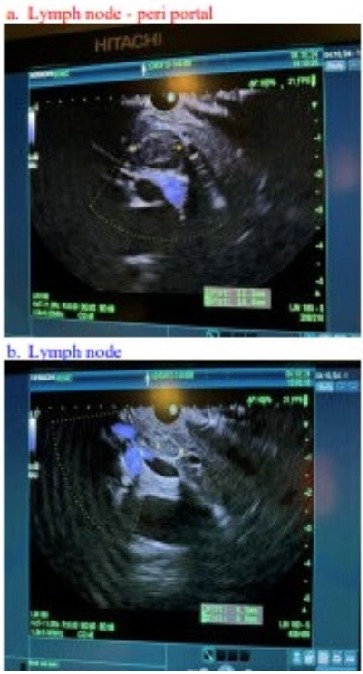
Figure: A. Peri-portal Lymph Node
B. Lymph Node
B. Lymph Node
Disclosures:
Raj Mohan Ram Mohan indicated no relevant financial relationships.
Leeza Pannikodu indicated no relevant financial relationships.
Sai Reshma Magam indicated no relevant financial relationships.
Sai Greeshma Magam indicated no relevant financial relationships.
Melvin Joy indicated no relevant financial relationships.
Dilman Natt indicated no relevant financial relationships.
Abhishek Tadikonda indicated no relevant financial relationships.
Winghang Lau indicated no relevant financial relationships.
Jiten Desai indicated no relevant financial relationships.
Paul Mustacchia indicated no relevant financial relationships.
Raj Mohan Ram Mohan, MD, Leeza Pannikodu, MD, Sai Reshma Magam, MD, Sai Greeshma Magam, MD, Melvin Joy, MD, Dilman Natt, MD, Abhishek Tadikonda, MD, Winghang Lau, MD, Jiten Desai, MD, Paul Mustacchia, MD, MBA. P0290 - Diagnostic Challenges and Effective Treatment of Gastrointestinal TB: Insights From a Clinical Case, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
