Sunday Poster Session
Category: Colon
P0293 - Gastrointestinal Amyloidosis: An Unusual Cause of Mesenteric Ischemia
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Malik Mushannen, MD
New York-Presbyterian / Brooklyn Methodist Hospital
Brooklyn, NY
Presenting Author(s)
Award: Presidential Poster Award
Malik Mushannen, MD1, Anas Zaher, MD1, Benjamin Gordon, MD2, Dana J. Lukin, MD3
1New York-Presbyterian / Brooklyn Methodist Hospital, Brooklyn, NY; 2New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 3Jill Roberts Center for Inflammatory Bowel Disease, New York Presbyterian Hospital-Weill Cornell Medicine, New York, NY
Introduction: While most cases of acute mesenteric ischemia are due to arterial emboli, secondary causes due to extrinsic vascular compromise of the mesenteric blood supply also exist (1). Here, we present a rare case of amyloidosis in a 76-year-old woman causing secondary mesenteric ischemia.
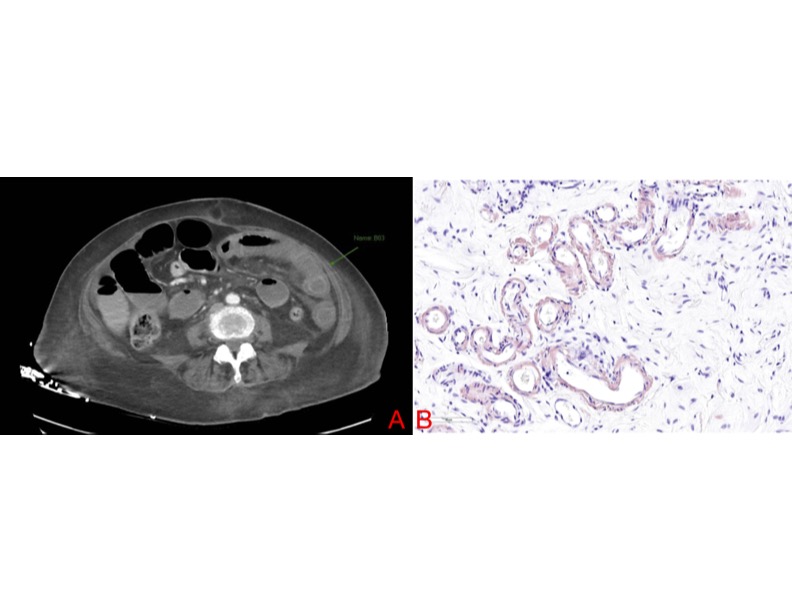
Case Description/Methods: A 76-year-old woman with rectal adenocarcinoma status post radiation, chemotherapy and resection, presented to the emergency department (ED) for three days of sharp, 8/10, non-radiating right upper quadrant abdominal pain. It was associated with nausea, non-bloody-non-bilious emesis, and decreased ostomy output. She was afebrile, tachycardic to 102 and hypotensive to 84/56. Physical exam revealed dry mucous membranes and distended abdomen with tenderness to palpation in the right upper quadrant. Labs revealed a white blood cell count of 9.81 x 10^3/uL, platelet count of 719 x 10^3/uL, sodium of 130 mEq/L, bicarbonate of 19 mEq/L, magnesium of 0.8 mg/dL, creatinine of 1.48 mg/dL, anion gap of 13 mEq/L, lactate of 2.3 mmol/L, and pH of 7.33 on venous blood gas. A CT abdomen and pelvis with intravenous contrast revealed edematous, hypoenhancing loops of small bowel in the left abdomen, suspicious for ischemic bowel, as well as dilated small bowel both proximal and distal to the suspected ischemic area (figure A). The patient underwent an emergent exploratory laparotomy, revealing suspected peritoneal carcinomatosis, recurrent pelvic side wall tumor, bowel dilation without intestinal necrosis, 50 cm of small bowel tethered to the pelvic sidewall encased in possible tumor, and one small area of sealed perforation in the small bowel. The pathology samples surprisingly were positive for amyloidosis, showing apple-green birefringence on Congo staining (Figure B), and no evidence of malignancy. The extent of amyloidosis included the mucosal vessels. Unfortunately, the patient’s post-operative course was complicated by septic shock, and she expired.
Discussion: While this case demonstrates a classic presentation of mesenteric ischemia, the underlying etiology of amyloidosis is rarely reported. Gastrointestinal amyloidosis typically involves infiltration of the mucosa causing malabsorption and diarrhea. Evidently, this was not the case of our patient, as her amyloidosis had infiltrated the vasculature of the bowel, restricting blood supply to the intestines. This patient had secondary amyloid due to her metastatic cancer which caused secondary acute mesenteric ischemia (3).
Disclosures:
Malik Mushannen, MD1, Anas Zaher, MD1, Benjamin Gordon, MD2, Dana J. Lukin, MD3. P0293 - Gastrointestinal Amyloidosis: An Unusual Cause of Mesenteric Ischemia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Malik Mushannen, MD1, Anas Zaher, MD1, Benjamin Gordon, MD2, Dana J. Lukin, MD3
1New York-Presbyterian / Brooklyn Methodist Hospital, Brooklyn, NY; 2New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 3Jill Roberts Center for Inflammatory Bowel Disease, New York Presbyterian Hospital-Weill Cornell Medicine, New York, NY
Introduction: While most cases of acute mesenteric ischemia are due to arterial emboli, secondary causes due to extrinsic vascular compromise of the mesenteric blood supply also exist (1). Here, we present a rare case of amyloidosis in a 76-year-old woman causing secondary mesenteric ischemia.
Case Description/Methods: A 76-year-old woman with rectal adenocarcinoma status post radiation, chemotherapy and resection, presented to the emergency department (ED) for three days of sharp, 8/10, non-radiating right upper quadrant abdominal pain. It was associated with nausea, non-bloody-non-bilious emesis, and decreased ostomy output. She was afebrile, tachycardic to 102 and hypotensive to 84/56. Physical exam revealed dry mucous membranes and distended abdomen with tenderness to palpation in the right upper quadrant. Labs revealed a white blood cell count of 9.81 x 10^3/uL, platelet count of 719 x 10^3/uL, sodium of 130 mEq/L, bicarbonate of 19 mEq/L, magnesium of 0.8 mg/dL, creatinine of 1.48 mg/dL, anion gap of 13 mEq/L, lactate of 2.3 mmol/L, and pH of 7.33 on venous blood gas. A CT abdomen and pelvis with intravenous contrast revealed edematous, hypoenhancing loops of small bowel in the left abdomen, suspicious for ischemic bowel, as well as dilated small bowel both proximal and distal to the suspected ischemic area (figure A). The patient underwent an emergent exploratory laparotomy, revealing suspected peritoneal carcinomatosis, recurrent pelvic side wall tumor, bowel dilation without intestinal necrosis, 50 cm of small bowel tethered to the pelvic sidewall encased in possible tumor, and one small area of sealed perforation in the small bowel. The pathology samples surprisingly were positive for amyloidosis, showing apple-green birefringence on Congo staining (Figure B), and no evidence of malignancy. The extent of amyloidosis included the mucosal vessels. Unfortunately, the patient’s post-operative course was complicated by septic shock, and she expired.
Discussion: While this case demonstrates a classic presentation of mesenteric ischemia, the underlying etiology of amyloidosis is rarely reported. Gastrointestinal amyloidosis typically involves infiltration of the mucosa causing malabsorption and diarrhea. Evidently, this was not the case of our patient, as her amyloidosis had infiltrated the vasculature of the bowel, restricting blood supply to the intestines. This patient had secondary amyloid due to her metastatic cancer which caused secondary acute mesenteric ischemia (3).
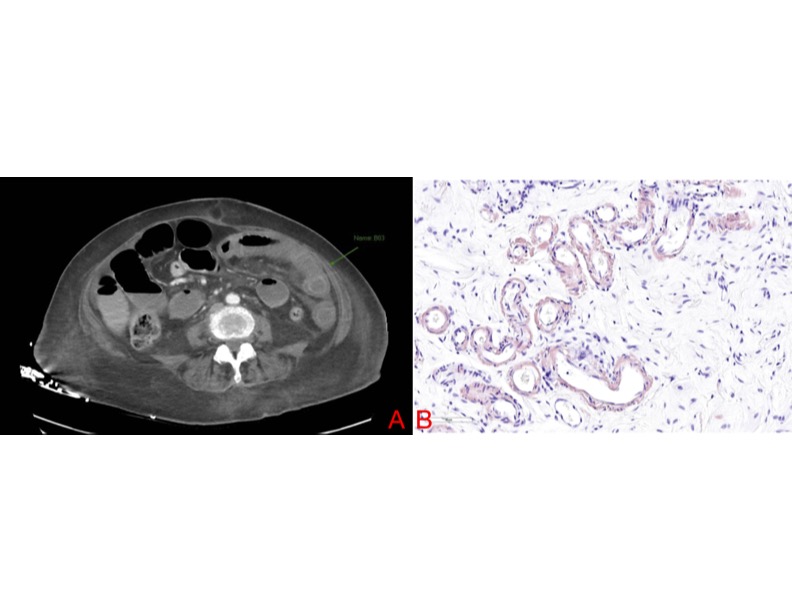
Figure: Figure A: CTAP showing edematous, hypoenhancing loops of small bowel in the left abdomen, suspicious for ischemic bowel.
Figure B: Pathology slide showing submucosal vessels staining positive on Congo red stain along the vessel walls with vessel wall thickening
Figure B: Pathology slide showing submucosal vessels staining positive on Congo red stain along the vessel walls with vessel wall thickening
Disclosures:
Malik Mushannen indicated no relevant financial relationships.
Anas Zaher indicated no relevant financial relationships.
Benjamin Gordon indicated no relevant financial relationships.
Dana J. Lukin: AbbVie – Consultant, Grant/Research Support, Speakers Bureau. AltruBio – Consultant. Boehringer Ingelheim – Consultant, Grant/Research Support. Bristol Myers Squibb – Consultant. Eli Lilly – Consultant. Fresenius Kabi – Consultant. Janssen – Consultant, Grant/Research Support, Speakers Bureau. Magellan Health – Consultant. Palatin Technologies – Consultant. Pfizer – Consultant. Prometheus Laboratories – Consultant. PSI – Consultant. Takeda – Consultant, Grant/Research Support.
Malik Mushannen, MD1, Anas Zaher, MD1, Benjamin Gordon, MD2, Dana J. Lukin, MD3. P0293 - Gastrointestinal Amyloidosis: An Unusual Cause of Mesenteric Ischemia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

