Sunday Poster Session
Category: Colon
P0298 - Unmasking the Silent Invader: Tuberculosis Colitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Sakshi Bai, MD,
Henry Ford Jackson Hospital
Jackson, MI
Presenting Author(s)
Sakshi Bai, MD,1, Bipneet Singh, MD1, Jahnavi Ethakota, MD1, Huma Tariq, MD1, Akhil Rahman, MD2
1Henry Ford Jackson Hospital, Jackson, MI; 2Henry Ford Jackson Hospital, Ann Arbor, MI
Introduction: Gastrointestinal tuberculosis (TB) is a prominent form of extrapulmonary TB that presents diagnostic challenges due to symptom overlap with other gastrointestinal conditions and the limited accuracy of current diagnostic tests. There is a critical need for increased awareness of this disease, particularly in regions with low disease prevalence such as developed countries. Left untreated, gastrointestinal TB can result in considerable morbidity, requiring prolonged hospital stays and sometimes surgical intervention. Early and accurate diagnosis followed by prompt initiation of therapy is crucial in preventing these complications. This detailed case study focuses on TB colitis, highlighting its clinical features, diagnostic approaches, and management protocol of extended drug resistant tuberculosis.
Case Description/Methods: We present the case of a 36-year-old immigrant from Honduras who initially presented with rectal bleeding, night sweats, and a notable weight loss of 30 pounds over 8 weeks. Colonoscopy identified Acid-fast bacilli (AFB)-positive granulomatous colitis, prompting a multidisciplinary diagnostic approach that included imaging studies, colonoscopy and microbiological confirmation.
Discussion: This case underscores the importance of considering tuberculosis (TB) in the differential diagnosis of gastrointestinal symptoms. TB can affect the digestive tract, presenting similarly to conditions like Crohn's disease. Colonoscopy with deep biopsy is crucial for tissue diagnosis, revealing characteristic ulcerative and hypertrophic lesions.
Polymerase chain reaction (PCR) significantly enhances diagnostic sensitivity and specificity compared to traditional methods. Treatment involves anti-TB medication, with follow-up colonoscopy showing gut response within 3-4 weeks. Surgical intervention may be necessary for complications such as stricture formation.
Timely recognition and management are essential to prevent morbidity associated with TB colitis, especially in atypical presentations. Increasing clinician awareness is critical for improving diagnostic accuracy and ensuring prompt initiation of appropriate therapy.

Disclosures:
Sakshi Bai, MD,1, Bipneet Singh, MD1, Jahnavi Ethakota, MD1, Huma Tariq, MD1, Akhil Rahman, MD2. P0298 - Unmasking the Silent Invader: Tuberculosis Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Henry Ford Jackson Hospital, Jackson, MI; 2Henry Ford Jackson Hospital, Ann Arbor, MI
Introduction: Gastrointestinal tuberculosis (TB) is a prominent form of extrapulmonary TB that presents diagnostic challenges due to symptom overlap with other gastrointestinal conditions and the limited accuracy of current diagnostic tests. There is a critical need for increased awareness of this disease, particularly in regions with low disease prevalence such as developed countries. Left untreated, gastrointestinal TB can result in considerable morbidity, requiring prolonged hospital stays and sometimes surgical intervention. Early and accurate diagnosis followed by prompt initiation of therapy is crucial in preventing these complications. This detailed case study focuses on TB colitis, highlighting its clinical features, diagnostic approaches, and management protocol of extended drug resistant tuberculosis.
Case Description/Methods: We present the case of a 36-year-old immigrant from Honduras who initially presented with rectal bleeding, night sweats, and a notable weight loss of 30 pounds over 8 weeks. Colonoscopy identified Acid-fast bacilli (AFB)-positive granulomatous colitis, prompting a multidisciplinary diagnostic approach that included imaging studies, colonoscopy and microbiological confirmation.
Discussion: This case underscores the importance of considering tuberculosis (TB) in the differential diagnosis of gastrointestinal symptoms. TB can affect the digestive tract, presenting similarly to conditions like Crohn's disease. Colonoscopy with deep biopsy is crucial for tissue diagnosis, revealing characteristic ulcerative and hypertrophic lesions.
Polymerase chain reaction (PCR) significantly enhances diagnostic sensitivity and specificity compared to traditional methods. Treatment involves anti-TB medication, with follow-up colonoscopy showing gut response within 3-4 weeks. Surgical intervention may be necessary for complications such as stricture formation.
Timely recognition and management are essential to prevent morbidity associated with TB colitis, especially in atypical presentations. Increasing clinician awareness is critical for improving diagnostic accuracy and ensuring prompt initiation of appropriate therapy.

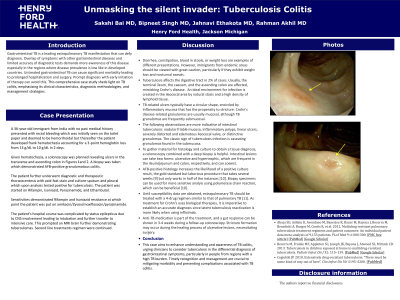
Figure: Ulcer in transverse Colon
Disclosures:
Sakshi Bai indicated no relevant financial relationships.
Bipneet Singh indicated no relevant financial relationships.
Jahnavi Ethakota indicated no relevant financial relationships.
Huma Tariq indicated no relevant financial relationships.
Akhil Rahman indicated no relevant financial relationships.
Sakshi Bai, MD,1, Bipneet Singh, MD1, Jahnavi Ethakota, MD1, Huma Tariq, MD1, Akhil Rahman, MD2. P0298 - Unmasking the Silent Invader: Tuberculosis Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
