Sunday Poster Session
Category: Colon
P0300 - Beating the Odds: Unusual Early Diagnosis of Primary Rectal Melanoma
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Rishika Trivedi, MD
DHR Health
Edinburg, TX
Presenting Author(s)
Rishika Trivedi, MD1, Mahmoud Barbarawi, MD2, Asif Zamir, MD, FACG2
1DHR Health, Edinburg, TX; 2DHR Health Gastroenterology, Edinburg, TX
Introduction: Rectal melanoma is an extremely rare malignancy, accounting for 4% of anorectal malignancies and less than 1% of all melanomas. It commonly occurs in females, with 54–76% occurring between the fifth and sixth decade of life. Due to its aggressive nature, its 5-year survival rate remains 10–20%. Early diagnosis is difficult due to its rarity and nonspecific symptoms.
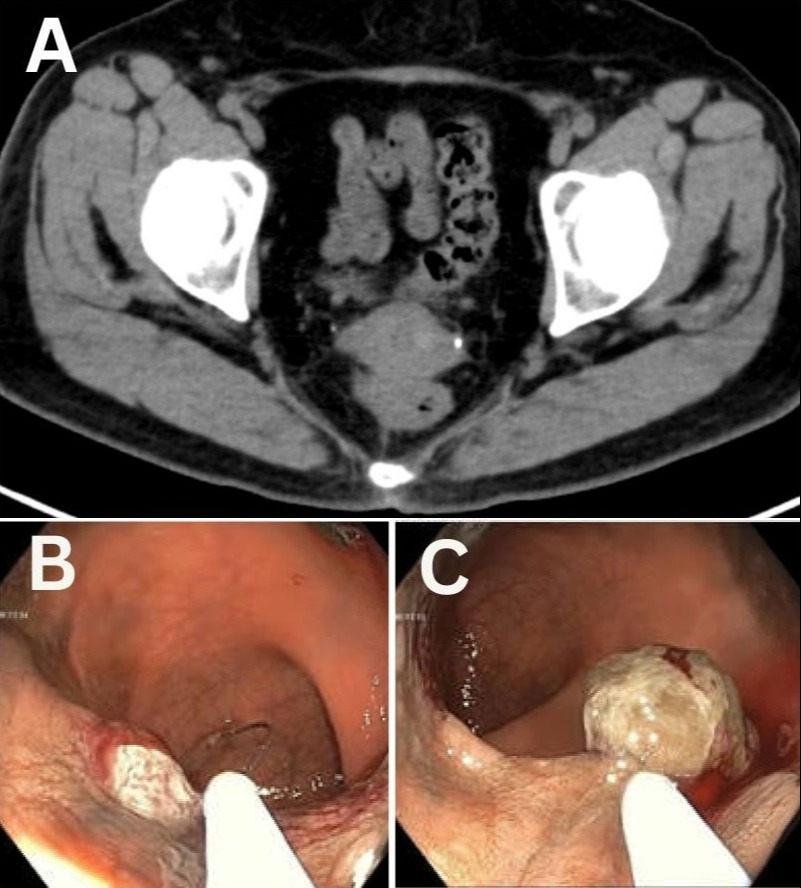
Case Description/Methods: A 64-year-old Hispanic female with a history of cholecystectomy and diabetes was referred for evaluation of intermittent right upper quadrant pain ongoing for four months. The initial laboratory tests and CT scan of abdomen/pelvis were unremarkable (Figure A). Due to persistent symptoms an EGD and colonoscopy were performed. Colonoscopy revealed distal rectal polyp measuring 1 cm in size (Figure B,C). Polypectomy was performed, and the pathology report confirmed mucosal-pigmented malignant melanoma with greatest depth of invasion of 0.8 mm. Immunohistochemical stains were positive for S-100, SOX-10, HMB-45, Melan A, and PRAME, and negative for BRAF, V600E, AE1/AE3, and CD68. The patient had no personal or family history of cutaneous melanoma. Whole-body PET showed no evidence of metastasis. The patient was started on immunotherapy with nivolumab. Flexible sigmoidoscopy with endoscopic ultrasound revealed a rectal scar and enlarged perirectal lymph nodes. A biopsy of the rectal scar was negative for granulomas, dysplasia, or malignancy. After 6 months of follow-up, the workup showed no signs of disease progression or metastasis.
Discussion: This case highlights primary rectal melanoma, an exceedingly rare and aggressive malignancy. At the time of diagnosis, 28-35% of the patients present with metastasis of the tumor, however this case was detected early. In case of diagnostic difficulty, immunohistochemical staining using antigens is crucial. The mainstay of the treatment is surgical resection with wide local excision or abdominoperineal resection. Further treatment strategies include chemotherapy, immunotherapy and targeted therapy. A high index of suspicion and prompt diagnosis along with a multidisciplinary approach are fundamental for improving the patient outcome.
Disclosures:
Rishika Trivedi, MD1, Mahmoud Barbarawi, MD2, Asif Zamir, MD, FACG2. P0300 - Beating the Odds: Unusual Early Diagnosis of Primary Rectal Melanoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1DHR Health, Edinburg, TX; 2DHR Health Gastroenterology, Edinburg, TX
Introduction: Rectal melanoma is an extremely rare malignancy, accounting for 4% of anorectal malignancies and less than 1% of all melanomas. It commonly occurs in females, with 54–76% occurring between the fifth and sixth decade of life. Due to its aggressive nature, its 5-year survival rate remains 10–20%. Early diagnosis is difficult due to its rarity and nonspecific symptoms.
Case Description/Methods: A 64-year-old Hispanic female with a history of cholecystectomy and diabetes was referred for evaluation of intermittent right upper quadrant pain ongoing for four months. The initial laboratory tests and CT scan of abdomen/pelvis were unremarkable (Figure A). Due to persistent symptoms an EGD and colonoscopy were performed. Colonoscopy revealed distal rectal polyp measuring 1 cm in size (Figure B,C). Polypectomy was performed, and the pathology report confirmed mucosal-pigmented malignant melanoma with greatest depth of invasion of 0.8 mm. Immunohistochemical stains were positive for S-100, SOX-10, HMB-45, Melan A, and PRAME, and negative for BRAF, V600E, AE1/AE3, and CD68. The patient had no personal or family history of cutaneous melanoma. Whole-body PET showed no evidence of metastasis. The patient was started on immunotherapy with nivolumab. Flexible sigmoidoscopy with endoscopic ultrasound revealed a rectal scar and enlarged perirectal lymph nodes. A biopsy of the rectal scar was negative for granulomas, dysplasia, or malignancy. After 6 months of follow-up, the workup showed no signs of disease progression or metastasis.
Discussion: This case highlights primary rectal melanoma, an exceedingly rare and aggressive malignancy. At the time of diagnosis, 28-35% of the patients present with metastasis of the tumor, however this case was detected early. In case of diagnostic difficulty, immunohistochemical staining using antigens is crucial. The mainstay of the treatment is surgical resection with wide local excision or abdominoperineal resection. Further treatment strategies include chemotherapy, immunotherapy and targeted therapy. A high index of suspicion and prompt diagnosis along with a multidisciplinary approach are fundamental for improving the patient outcome.
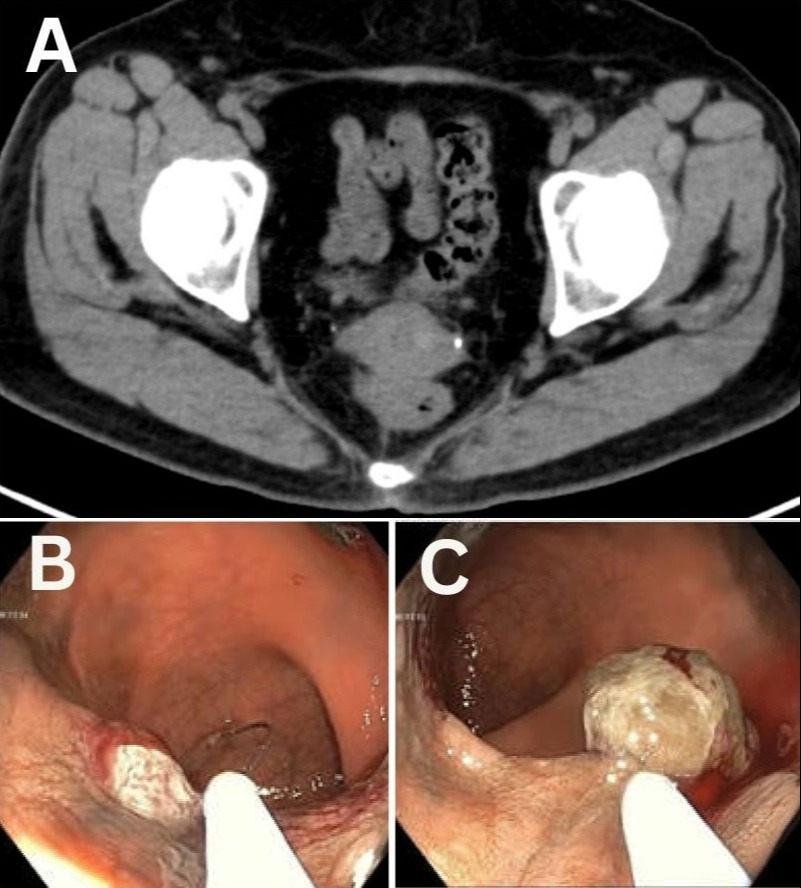
Figure: Figure: A: CT abdomen and pelvis axial view showing unremarkable findings. B and C: Colonoscopic views of the rectum showing polyp in the distal rectum.
Disclosures:
Rishika Trivedi indicated no relevant financial relationships.
Mahmoud Barbarawi indicated no relevant financial relationships.
Asif Zamir indicated no relevant financial relationships.
Rishika Trivedi, MD1, Mahmoud Barbarawi, MD2, Asif Zamir, MD, FACG2. P0300 - Beating the Odds: Unusual Early Diagnosis of Primary Rectal Melanoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
