Sunday Poster Session
Category: Colon
P0345 - A Case of Eosinophilic Granulomatosis With Polyangiitis With Initial Presentation of Colitis and Enteritis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- OM
Omar Mourad
Weill Cornell Medicine
Doha, Al Wakrah, Qatar
Presenting Author(s)
Omar Mourad, 1, Farha Shaikh, 2, Emily Smith, MD3, David Berlin, MD4, David Wan, MD5
1Weill Cornell Medicine, Doha, Al Wakrah, Qatar; 2Weill Cornell Medicine, Doha, Ad Dawhah, Qatar; 3New York-Presbyterian/Weill Cornell, New York, NY; 4New York-Presbyterian Hospital, New York, NY; 5New York-Presbyterian / Weill Cornell Medical Center, New York, NY
Introduction: Eosinophilic Granulomatosis with Polyangiitis (EGPA) is an anti-neutrophil cytoplasmic antibody (ANCA) positive vasculitis of small and medium arteries characterized by severe asthma, hypereosinophilia, extravascular granulomas, and necrotizing vasculitis. Patients typically report fever, weight loss, and fatigue with some experiencing multi-system involvement with cardiac, pulmonary, and upper respiratory symptoms. This case is a patient initially presenting to healthcare for respiratory symptoms, on dupixent, now presenting with abdominal pain, nausea, vomiting, and diarrhea.
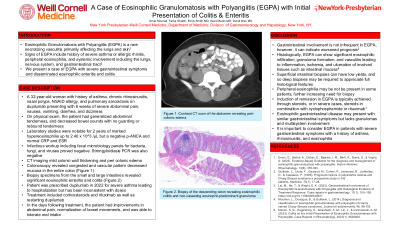
Case Description/Methods: A 32-year-old woman with history of asthma maintained on dupilimumab, chronic rhinosinusitis, nasal polyposis, sickle cell trait, prior provoked pulmonary embolism, and pulmonary sarcoidosis, presented with 6 weeks of abdominal pain, nausea, vomiting, and diarrhea. Exam was notable for diffuse abdominal tenderness with palpation without guarding or rebound, and decreased bowel sounds. Labs were notable for marked peripheral hypereosinophilia for 2 years up to 2.40 x103/μL and a negative p-ANCA. Abdominal imaging showed colonic wall thickening and pericolonic edema. Colonoscopy was performed showing diffuse vascular-pattern-decreased mucosa in the colon with scattered nodular mucosa in the terminal ileum. Biopsies revealed eosinophilic enterocolitis. Serum and stool infectious studies were negative. Differentials included autoimmune conditions such as EGPA, Crohn’s disease, and medication induced injury. Given mucosal distribution of infiltrative eosinophils within the intestine, history of nasal polyps with eosinophilic infiltration, and refractory asthma, the diagnosis of seronegative EGPA was made.
Discussion: There is no verified diagnostic criteria for EGPA. Diagnosis is based on clinical findings (such as obstructive airway disease, nasal polyps, and mononeuritis multiplex) with eosinophilia, p-ANCA positivity, and biopsy showing extravascular eosinophilic-predominant inflammation. On histology, seronegative EGPA is less likely to have a vasculitic picture that is seen in vasculitides (such as in seropositive EGPA). EGPA should be considered in patients with a history of asthma, chronic rhinosinusitis with polyps, and chronic peripheral eosinophilia with end organ involvement. This patient arrived in the ED with severe abdominal pain with chronic diarrhea. She was found on colonoscopy to have eosinophilic enterocolitis. Early gastrointestinal involvement is an uncommon presentation in EGPA.
Disclosures:
Omar Mourad, 1, Farha Shaikh, 2, Emily Smith, MD3, David Berlin, MD4, David Wan, MD5. P0345 - A Case of Eosinophilic Granulomatosis With Polyangiitis With Initial Presentation of Colitis and Enteritis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Weill Cornell Medicine, Doha, Al Wakrah, Qatar; 2Weill Cornell Medicine, Doha, Ad Dawhah, Qatar; 3New York-Presbyterian/Weill Cornell, New York, NY; 4New York-Presbyterian Hospital, New York, NY; 5New York-Presbyterian / Weill Cornell Medical Center, New York, NY
Introduction: Eosinophilic Granulomatosis with Polyangiitis (EGPA) is an anti-neutrophil cytoplasmic antibody (ANCA) positive vasculitis of small and medium arteries characterized by severe asthma, hypereosinophilia, extravascular granulomas, and necrotizing vasculitis. Patients typically report fever, weight loss, and fatigue with some experiencing multi-system involvement with cardiac, pulmonary, and upper respiratory symptoms. This case is a patient initially presenting to healthcare for respiratory symptoms, on dupixent, now presenting with abdominal pain, nausea, vomiting, and diarrhea.
Case Description/Methods: A 32-year-old woman with history of asthma maintained on dupilimumab, chronic rhinosinusitis, nasal polyposis, sickle cell trait, prior provoked pulmonary embolism, and pulmonary sarcoidosis, presented with 6 weeks of abdominal pain, nausea, vomiting, and diarrhea. Exam was notable for diffuse abdominal tenderness with palpation without guarding or rebound, and decreased bowel sounds. Labs were notable for marked peripheral hypereosinophilia for 2 years up to 2.40 x103/μL and a negative p-ANCA. Abdominal imaging showed colonic wall thickening and pericolonic edema. Colonoscopy was performed showing diffuse vascular-pattern-decreased mucosa in the colon with scattered nodular mucosa in the terminal ileum. Biopsies revealed eosinophilic enterocolitis. Serum and stool infectious studies were negative. Differentials included autoimmune conditions such as EGPA, Crohn’s disease, and medication induced injury. Given mucosal distribution of infiltrative eosinophils within the intestine, history of nasal polyps with eosinophilic infiltration, and refractory asthma, the diagnosis of seronegative EGPA was made.
Discussion: There is no verified diagnostic criteria for EGPA. Diagnosis is based on clinical findings (such as obstructive airway disease, nasal polyps, and mononeuritis multiplex) with eosinophilia, p-ANCA positivity, and biopsy showing extravascular eosinophilic-predominant inflammation. On histology, seronegative EGPA is less likely to have a vasculitic picture that is seen in vasculitides (such as in seropositive EGPA). EGPA should be considered in patients with a history of asthma, chronic rhinosinusitis with polyps, and chronic peripheral eosinophilia with end organ involvement. This patient arrived in the ED with severe abdominal pain with chronic diarrhea. She was found on colonoscopy to have eosinophilic enterocolitis. Early gastrointestinal involvement is an uncommon presentation in EGPA.
Disclosures:
Omar Mourad indicated no relevant financial relationships.
Farha Shaikh indicated no relevant financial relationships.
Emily Smith indicated no relevant financial relationships.
David Berlin indicated no relevant financial relationships.
David Wan indicated no relevant financial relationships.
Omar Mourad, 1, Farha Shaikh, 2, Emily Smith, MD3, David Berlin, MD4, David Wan, MD5. P0345 - A Case of Eosinophilic Granulomatosis With Polyangiitis With Initial Presentation of Colitis and Enteritis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
