Sunday Poster Session
Category: Colon
P0347 - A Case of Lymphogranuloma Venereum Proctitis Mimicking Rectal Malignancy
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E

Abdullah A. Memon, MD
University of Illinois College of Medicine
Chicago, IL
Presenting Author(s)
Abdullah Memon, MD1, Sean C. Tompkins, MD, PhD2, Gabriela Mendez, MD1, Asim Shuja, MD3
1University of Illinois College of Medicine, Chicago, IL; 2University of Illinois, Chicago, IL; 3University of Illinois, Oak Park, IL
Introduction: Proctitis, or inflammation of the rectum, can have various etiologies, such as infection. This includes sexually transmitted diseases (STIs), especially in men who have sex with men (MSM), which typically present with rectal pain, bleeding and purulent discharge. Rectal malignancies can also have these symptoms, as well as weight loss. We present a case of a patient with a known rectal mass, initially thought to be a malignancy, but after further workup was attributed to lymphogranuloma venereum (LGV) proctitis.
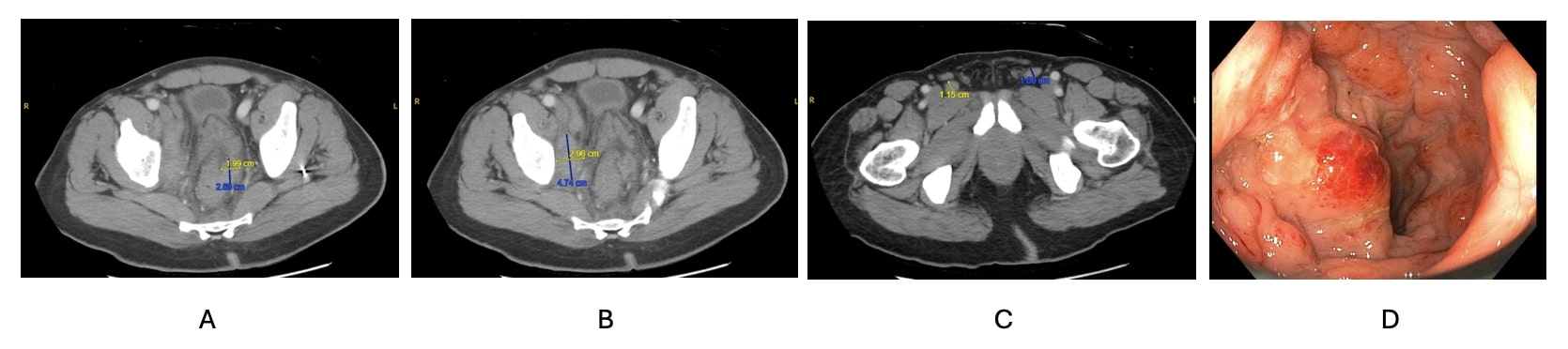
Case Description/Methods: A 52 year-old male with past medical history of rectal STIs presented with rectal pain, hematochezia, and a 40 lb weight loss over 2 months. He was seen at two other emergency departments in the 2 months prior, both with CT reads concerning for metastatic malignancy. HIV testing was negative on admission. CT abdomen/pelvis showed diffuse wall thickening of the rectum with perirectal stranding along with iliac chain and inguinal lymphadenopathy. Colonoscopy revealed congested, erythematous and nodular mucosa in the rectum that was more consistent with a solitary rectal ulcer as opposed to malignancy. Biopsy was notable for nodular tubuloglandular mucosa with marked ongoing inflammation within the lamina propria, negative for high grade dysplasia and malignancy. In addition, Giemsa stain was inconclusive for chlamydia. Rectal swab, however, was positive for chlamydia, and LGV proctitis was thought to be the most likely etiology for the patient’s symptoms. He was prescribed a 21-day course of doxycycline, after which he was completely asymptomatic.
Discussion: LGV is an STI caused by the L1, L2, and L3 serovars of chlamydia trachomatis, which in the past two decades has been presenting as proctitis in MSM in Western Europe and North America. Primary infection is characterized by a genital ulcer at the site of inoculation, with a period of 3-12 days, that spontaneously heals. Secondary LGV, occurring 2-6 weeks after initial exposure, includes lymphatic involvement and manifests as anorectal syndrome. Tertiary LGV involves fibrosis and strictures due to lack of treatment. In our case, colon biopsies were insufficient to make the diagnosis of chlamydia proctitis as the diagnosis was made based on results of the rectal chlamydia swab. This highlights the importance of having LGV on the differential when ruling out rectal malignancy during a colonoscopy, so appropriate diagnostic tests are performed, as delayed or no treatment can lead to irreversible sequelae.
Disclosures:
Abdullah Memon, MD1, Sean C. Tompkins, MD, PhD2, Gabriela Mendez, MD1, Asim Shuja, MD3. P0347 - A Case of Lymphogranuloma Venereum Proctitis Mimicking Rectal Malignancy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Illinois College of Medicine, Chicago, IL; 2University of Illinois, Chicago, IL; 3University of Illinois, Oak Park, IL
Introduction: Proctitis, or inflammation of the rectum, can have various etiologies, such as infection. This includes sexually transmitted diseases (STIs), especially in men who have sex with men (MSM), which typically present with rectal pain, bleeding and purulent discharge. Rectal malignancies can also have these symptoms, as well as weight loss. We present a case of a patient with a known rectal mass, initially thought to be a malignancy, but after further workup was attributed to lymphogranuloma venereum (LGV) proctitis.
Case Description/Methods: A 52 year-old male with past medical history of rectal STIs presented with rectal pain, hematochezia, and a 40 lb weight loss over 2 months. He was seen at two other emergency departments in the 2 months prior, both with CT reads concerning for metastatic malignancy. HIV testing was negative on admission. CT abdomen/pelvis showed diffuse wall thickening of the rectum with perirectal stranding along with iliac chain and inguinal lymphadenopathy. Colonoscopy revealed congested, erythematous and nodular mucosa in the rectum that was more consistent with a solitary rectal ulcer as opposed to malignancy. Biopsy was notable for nodular tubuloglandular mucosa with marked ongoing inflammation within the lamina propria, negative for high grade dysplasia and malignancy. In addition, Giemsa stain was inconclusive for chlamydia. Rectal swab, however, was positive for chlamydia, and LGV proctitis was thought to be the most likely etiology for the patient’s symptoms. He was prescribed a 21-day course of doxycycline, after which he was completely asymptomatic.
Discussion: LGV is an STI caused by the L1, L2, and L3 serovars of chlamydia trachomatis, which in the past two decades has been presenting as proctitis in MSM in Western Europe and North America. Primary infection is characterized by a genital ulcer at the site of inoculation, with a period of 3-12 days, that spontaneously heals. Secondary LGV, occurring 2-6 weeks after initial exposure, includes lymphatic involvement and manifests as anorectal syndrome. Tertiary LGV involves fibrosis and strictures due to lack of treatment. In our case, colon biopsies were insufficient to make the diagnosis of chlamydia proctitis as the diagnosis was made based on results of the rectal chlamydia swab. This highlights the importance of having LGV on the differential when ruling out rectal malignancy during a colonoscopy, so appropriate diagnostic tests are performed, as delayed or no treatment can lead to irreversible sequelae.
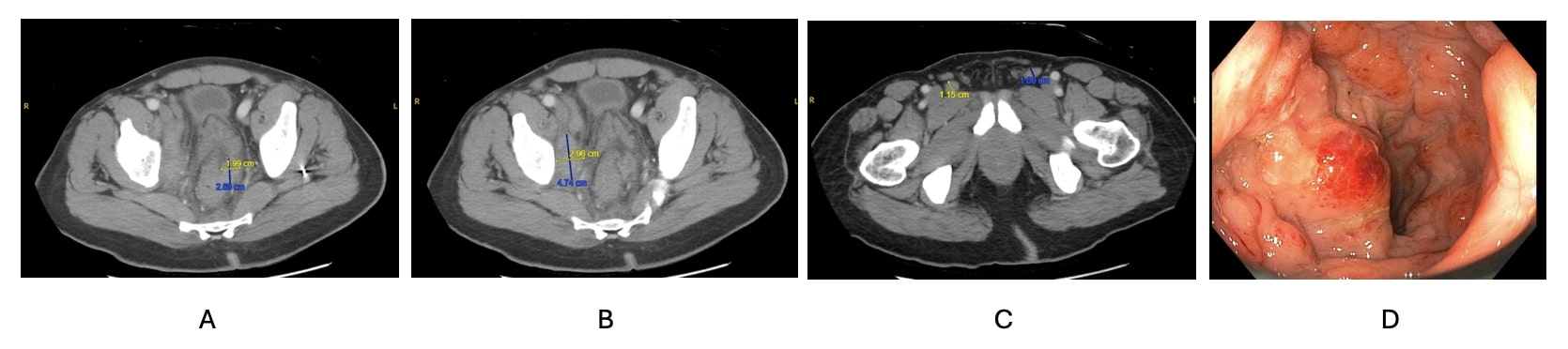
Figure: A. Diffuse rectal wall thickening and perirectal implants in the mesorectal fat, with one lesion measuring 2.7 x 2 cm. B. Conglomerate lymph nodes involving the right pelvic wall measuring 4.7 x 3 cm along the right external iliac chain. C. Mildly enlarged left inguinal lymph node measuring 1 cm in short axis and right inguinal lymph nodes measuring 1.2 cm in short axis. D. Congested, erythematous and nodular mucosa in the rectum as seen during colonoscopy.
Disclosures:
Abdullah Memon indicated no relevant financial relationships.
Sean Tompkins indicated no relevant financial relationships.
Gabriela Mendez indicated no relevant financial relationships.
Asim Shuja indicated no relevant financial relationships.
Abdullah Memon, MD1, Sean C. Tompkins, MD, PhD2, Gabriela Mendez, MD1, Asim Shuja, MD3. P0347 - A Case of Lymphogranuloma Venereum Proctitis Mimicking Rectal Malignancy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
