Sunday Poster Session
Category: Colorectal Cancer Prevention
P0405 - Open Access Colonoscopy: Assessing the Outcomes of a Novel Electronic Medical Record Best Practice Alert (BPA) in Reducing Inappropriate Colonoscopy Referrals
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Suhaib Alhaj Ali, MD
Henry Ford Hospital
Detroit, MI
Presenting Author(s)
Suhib Alhaj Ali, MD1, Omar Shamaa, MD2, Haya Omeish, MD2, Keith Mullins, MD1, Danielle Heidemann, MD1
1Henry Ford Hospital, Detroit, MI; 2Henry Ford Health, Detroit, MI
Introduction: In our prior study, we established that open access colonoscopy (OAC) for colon cancer screening is burdened by high inappropriate referral rates, leading to delayed patient care, increased resource use, & lower colonoscopy completion rates for rejected patients. Our group initiated a quality improvement project involving an electronic medical record (EMR) best practice alert (BPA) that notifies providers if specific criteria prohibiting OAC are met. This study assesses the BPA's outcomes after implementation.
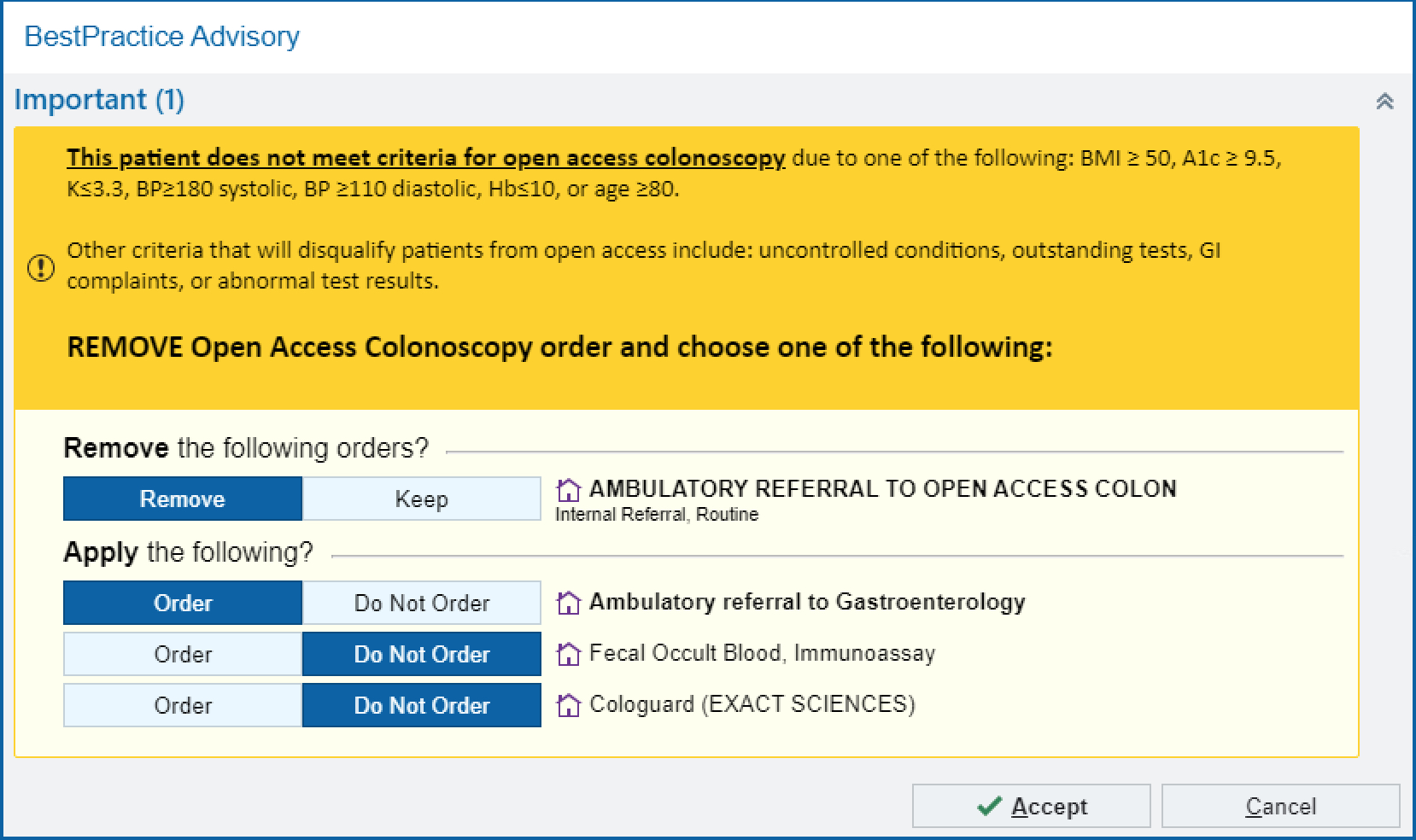
Methods: Starting April 2023, an EMR BPA was launched at our primary care clinic. Upon ordering OAC, if a patient meets prohibitive criteria, the BPA (seen in Fig. 1) notifies the provider to cancel the order & either refer to gastroenterology (GI) or order stool testing. If the order remains, a text box appears for an optional explanation. High-risk patients have only the GI referral option. Concurrently, we liberalized OAC guidelines, raising hemoglobin A1c (HbA1C) & body mass index (BMI) thresholds. Data from January to March 2024 was collected post-BPA refinement, & a random sample of 200 patients was chart reviewed to assess outcomes.
Results: From January to March 2024, the BPA was triggered 508 times. Mean age was 61.1 years. Common BPA triggers were hypokalemia ≤3.3 mmol/L (18.5%), HbA1C ≥9.5% (18.5%), hemoglobin ≤10 g/dL (15.5%), age ≥80 years (15.5%), BMI ≥50 kg/m2 (13.5%), & blood pressure ≥180/110 (8%). Most common alternatives were referral to GI (53%), stool testing (2%), or neither (45%). Those who ordered neither mostly proceeded with the order without any reason/changes (54.4%), or canceled it (24.4%). For “high risk” patients where the BPA triggered (n=51), only 52.9% were referred to GI. There were 5 cases where the BPA inaccurately fired, 19 cases where OAC referral was still accepted by GI despite BPA accuracy, & 20 cases where referral was rejected for another individualized reason. Only 11% of the sample completed any colon cancer screening & 9% completed a colonoscopy; mean time from referral to colonoscopy was 77.1 days.
Discussion: The BPA appears to reduce inappropriate referrals but effectiveness is limited by provider awareness & inability to factor in personalized patient factors. Low completion rates may be due to demographic challenges like missed appointments or socioeconomic barriers, as well as the recent nature of the data. This suggests a need for longer BPA implementation to fully assess its impact on referral appropriateness & completion rates.
Disclosures:
Suhib Alhaj Ali, MD1, Omar Shamaa, MD2, Haya Omeish, MD2, Keith Mullins, MD1, Danielle Heidemann, MD1. P0405 - Open Access Colonoscopy: Assessing the Outcomes of a Novel Electronic Medical Record Best Practice Alert (BPA) in Reducing Inappropriate Colonoscopy Referrals, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Henry Ford Hospital, Detroit, MI; 2Henry Ford Health, Detroit, MI
Introduction: In our prior study, we established that open access colonoscopy (OAC) for colon cancer screening is burdened by high inappropriate referral rates, leading to delayed patient care, increased resource use, & lower colonoscopy completion rates for rejected patients. Our group initiated a quality improvement project involving an electronic medical record (EMR) best practice alert (BPA) that notifies providers if specific criteria prohibiting OAC are met. This study assesses the BPA's outcomes after implementation.
Methods: Starting April 2023, an EMR BPA was launched at our primary care clinic. Upon ordering OAC, if a patient meets prohibitive criteria, the BPA (seen in Fig. 1) notifies the provider to cancel the order & either refer to gastroenterology (GI) or order stool testing. If the order remains, a text box appears for an optional explanation. High-risk patients have only the GI referral option. Concurrently, we liberalized OAC guidelines, raising hemoglobin A1c (HbA1C) & body mass index (BMI) thresholds. Data from January to March 2024 was collected post-BPA refinement, & a random sample of 200 patients was chart reviewed to assess outcomes.
Results: From January to March 2024, the BPA was triggered 508 times. Mean age was 61.1 years. Common BPA triggers were hypokalemia ≤3.3 mmol/L (18.5%), HbA1C ≥9.5% (18.5%), hemoglobin ≤10 g/dL (15.5%), age ≥80 years (15.5%), BMI ≥50 kg/m2 (13.5%), & blood pressure ≥180/110 (8%). Most common alternatives were referral to GI (53%), stool testing (2%), or neither (45%). Those who ordered neither mostly proceeded with the order without any reason/changes (54.4%), or canceled it (24.4%). For “high risk” patients where the BPA triggered (n=51), only 52.9% were referred to GI. There were 5 cases where the BPA inaccurately fired, 19 cases where OAC referral was still accepted by GI despite BPA accuracy, & 20 cases where referral was rejected for another individualized reason. Only 11% of the sample completed any colon cancer screening & 9% completed a colonoscopy; mean time from referral to colonoscopy was 77.1 days.
Discussion: The BPA appears to reduce inappropriate referrals but effectiveness is limited by provider awareness & inability to factor in personalized patient factors. Low completion rates may be due to demographic challenges like missed appointments or socioeconomic barriers, as well as the recent nature of the data. This suggests a need for longer BPA implementation to fully assess its impact on referral appropriateness & completion rates.
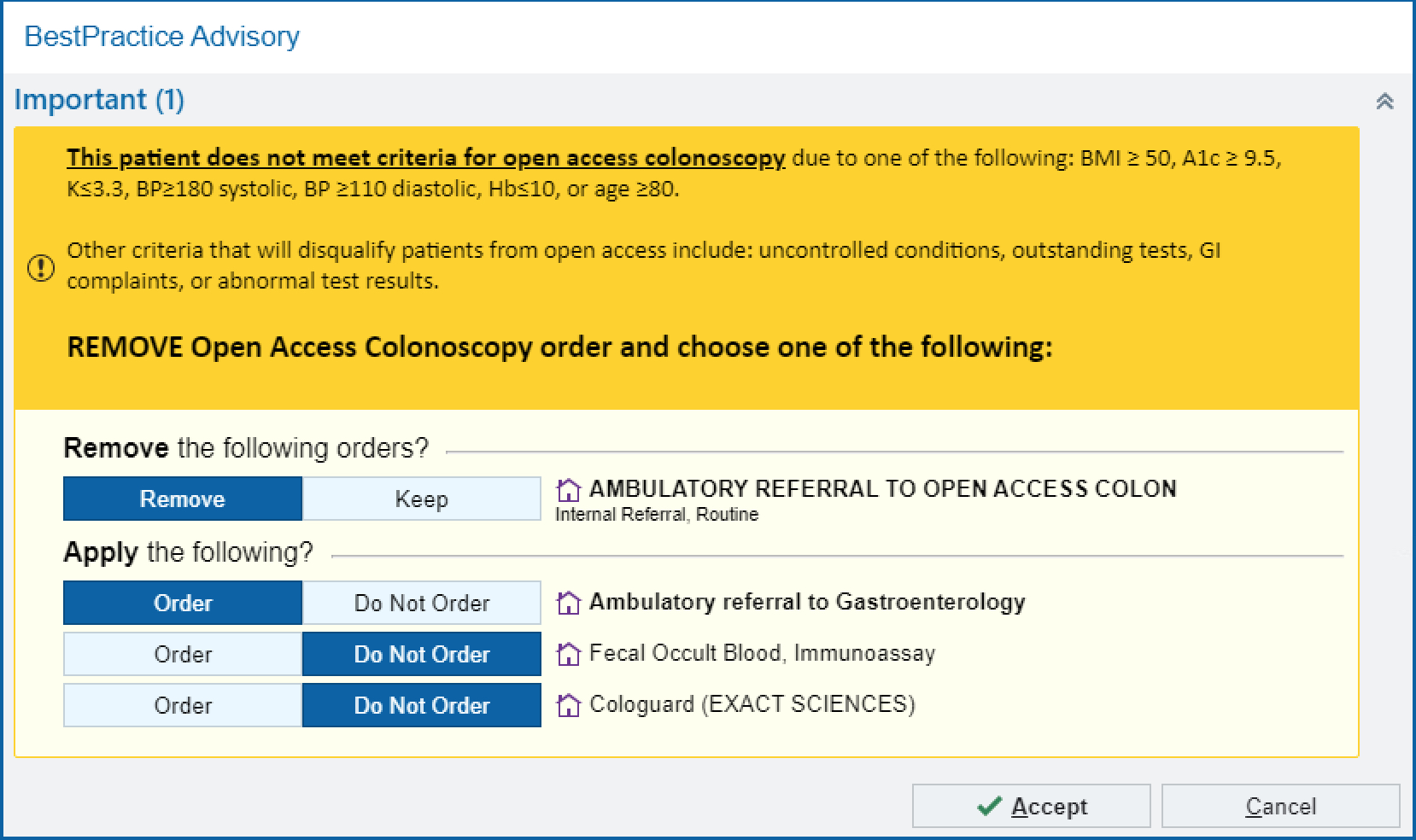
Figure: Fig. 1. BPA implemented in the primary care clinic at our tertiary center with options to keep or remove original OAC order, order an alternative (referral to gastroenterology and/or stool tests), or cancel the order altogether.
Disclosures:
Suhib Alhaj Ali indicated no relevant financial relationships.
Omar Shamaa indicated no relevant financial relationships.
Haya Omeish indicated no relevant financial relationships.
Keith Mullins indicated no relevant financial relationships.
Danielle Heidemann indicated no relevant financial relationships.
Suhib Alhaj Ali, MD1, Omar Shamaa, MD2, Haya Omeish, MD2, Keith Mullins, MD1, Danielle Heidemann, MD1. P0405 - Open Access Colonoscopy: Assessing the Outcomes of a Novel Electronic Medical Record Best Practice Alert (BPA) in Reducing Inappropriate Colonoscopy Referrals, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

