Sunday Poster Session
Category: Colorectal Cancer Prevention
P0411 - Colorectal Cancer Screening in 45-49 and 50-54-Year-Olds Detects Similar Rates of High-Risk Findings: Results From a U.S.-Wide Cloud-Based Data Set
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Michael S. Smith, MD, MBA
Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Michael S.. Smith, MD, MBA1, Stuart K. Amateau, MD, PhD, FACG2, Seth Gross, MD3, Nathan A.. Merriman, MD, MSCE4, Steve Serrao, MD5, Terry Bohlke, 6, Gregory Pepin, 7, Carol A.. Burke, MD, FACG8
1Icahn School of Medicine at Mount Sinai, New York, NY; 2University of Minnesota Medical Center, Minneapolis, MN; 3NYU Langone Health, New York, NY; 4Intermountain Health, Murray, UT; 5Riverside University Health System, Moreno Valley, CA; 6Community Health Systems, Franklin, TN; 7Provation, Minneapolis, MN; 8Digestive Disease Institute, Cleveland Clinic, Cleveland, OH
Introduction: Recent guidelines lowered the initial age for universal average-risk colorectal cancer (CRC) screening from 50 to 45 years, though not all societies have embraced this change. One expressed concern is a paucity of data showing a benefit of finding high-risk lesions in the younger cohort. The aim of this study was to compare lesion detection rates in patients meeting criteria for initial screening before and after guideline changes.
Methods: Provation Apex is an endoscopy documentation solution which stores procedure results in a HIPAA-compliant cloud database (Provation, Minneapolis, MN). Procedure data from previous software versions which utilized local storage also are migrated to the cloud, to be stored alongside newly documented exams. As new sites adopt Apex, their procedures are added to the cloud. With site consent, deidentified data can be aggregated to identify trends in procedure indications, findings and interventions. In 1/2024, all US colonoscopies from nearly 300 consenting sites were analyzed if a CRC screening indication was selected. Polyp detection was reviewed for two patient cohorts, representing the first years of the old and new recommended screening windows (ages 45-49 and 50-54). High risk findings were defined as the presence of a polyp at least 10 mm in diameter, or any mass lesion.
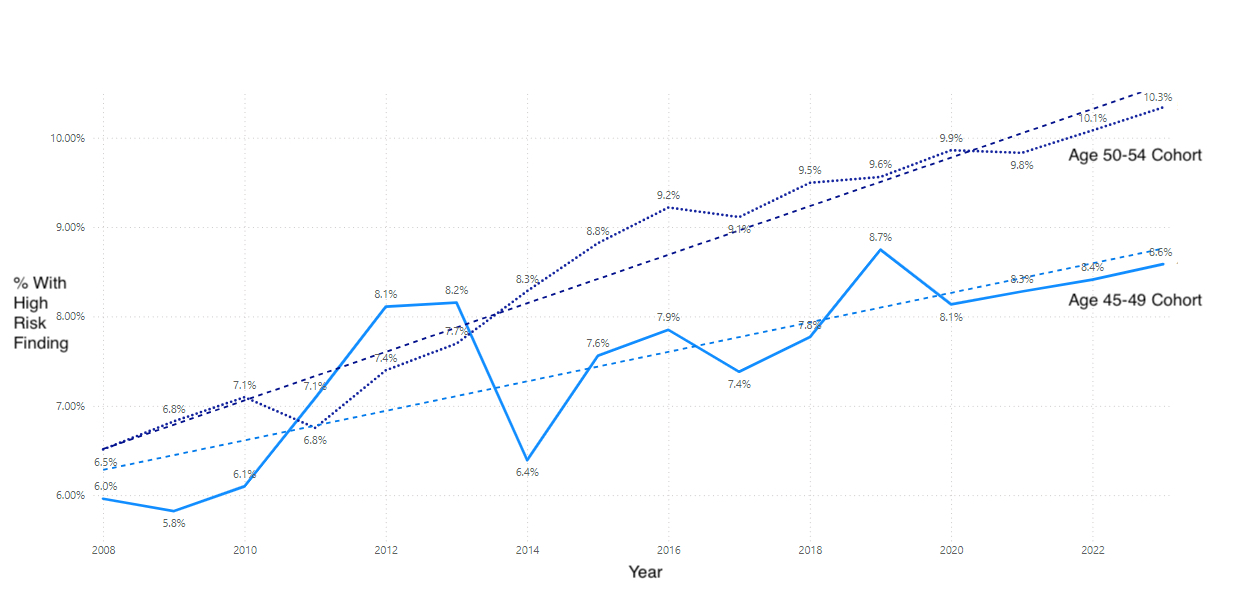
Results: Initial analysis focused on 2022-3, after GI society guidelines changed. During this period, CRC screening was performed on 101,822 45-49 year olds and 112,704 50-54 year olds (54% women). At least one polyp was found in 51.3% (ages 45-49) and 55.0% (ages 50-54) of exams, corresponding to estimated adenoma detection rates of 36.9% and 39.6%. Results from all 589,130 screening colonoscopies in the data set then were reviewed by year to identify trends. From 2008 to 2023, the proportion of exams with high risk findings increased in both cohorts, rising from 6.5% to 10.3% for ages 50-54, and from 6.0% to 8.6% for ages 45-49.
Discussion: There is a staggering increase in the number of high risk lesions detected during CRC screening colonoscopy over the study period for both cohorts, 59% for ages 50-54 and 44% for ages 45-49. By 2023, high risk lesion detection in the age 45-49 cohort reached the same rate the age 50-54 cohort had less than a decade before. These findings, plus a similar polyp detection rate in both groups, demonstrate the benefit of initiating CRC screening at ages 45-49 as high risk lesion detection rates continue to rise.
Disclosures:
Michael S.. Smith, MD, MBA1, Stuart K. Amateau, MD, PhD, FACG2, Seth Gross, MD3, Nathan A.. Merriman, MD, MSCE4, Steve Serrao, MD5, Terry Bohlke, 6, Gregory Pepin, 7, Carol A.. Burke, MD, FACG8. P0411 - Colorectal Cancer Screening in 45-49 and 50-54-Year-Olds Detects Similar Rates of High-Risk Findings: Results From a U.S.-Wide Cloud-Based Data Set, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Icahn School of Medicine at Mount Sinai, New York, NY; 2University of Minnesota Medical Center, Minneapolis, MN; 3NYU Langone Health, New York, NY; 4Intermountain Health, Murray, UT; 5Riverside University Health System, Moreno Valley, CA; 6Community Health Systems, Franklin, TN; 7Provation, Minneapolis, MN; 8Digestive Disease Institute, Cleveland Clinic, Cleveland, OH
Introduction: Recent guidelines lowered the initial age for universal average-risk colorectal cancer (CRC) screening from 50 to 45 years, though not all societies have embraced this change. One expressed concern is a paucity of data showing a benefit of finding high-risk lesions in the younger cohort. The aim of this study was to compare lesion detection rates in patients meeting criteria for initial screening before and after guideline changes.
Methods: Provation Apex is an endoscopy documentation solution which stores procedure results in a HIPAA-compliant cloud database (Provation, Minneapolis, MN). Procedure data from previous software versions which utilized local storage also are migrated to the cloud, to be stored alongside newly documented exams. As new sites adopt Apex, their procedures are added to the cloud. With site consent, deidentified data can be aggregated to identify trends in procedure indications, findings and interventions. In 1/2024, all US colonoscopies from nearly 300 consenting sites were analyzed if a CRC screening indication was selected. Polyp detection was reviewed for two patient cohorts, representing the first years of the old and new recommended screening windows (ages 45-49 and 50-54). High risk findings were defined as the presence of a polyp at least 10 mm in diameter, or any mass lesion.
Results: Initial analysis focused on 2022-3, after GI society guidelines changed. During this period, CRC screening was performed on 101,822 45-49 year olds and 112,704 50-54 year olds (54% women). At least one polyp was found in 51.3% (ages 45-49) and 55.0% (ages 50-54) of exams, corresponding to estimated adenoma detection rates of 36.9% and 39.6%. Results from all 589,130 screening colonoscopies in the data set then were reviewed by year to identify trends. From 2008 to 2023, the proportion of exams with high risk findings increased in both cohorts, rising from 6.5% to 10.3% for ages 50-54, and from 6.0% to 8.6% for ages 45-49.
Discussion: There is a staggering increase in the number of high risk lesions detected during CRC screening colonoscopy over the study period for both cohorts, 59% for ages 50-54 and 44% for ages 45-49. By 2023, high risk lesion detection in the age 45-49 cohort reached the same rate the age 50-54 cohort had less than a decade before. These findings, plus a similar polyp detection rate in both groups, demonstrate the benefit of initiating CRC screening at ages 45-49 as high risk lesion detection rates continue to rise.
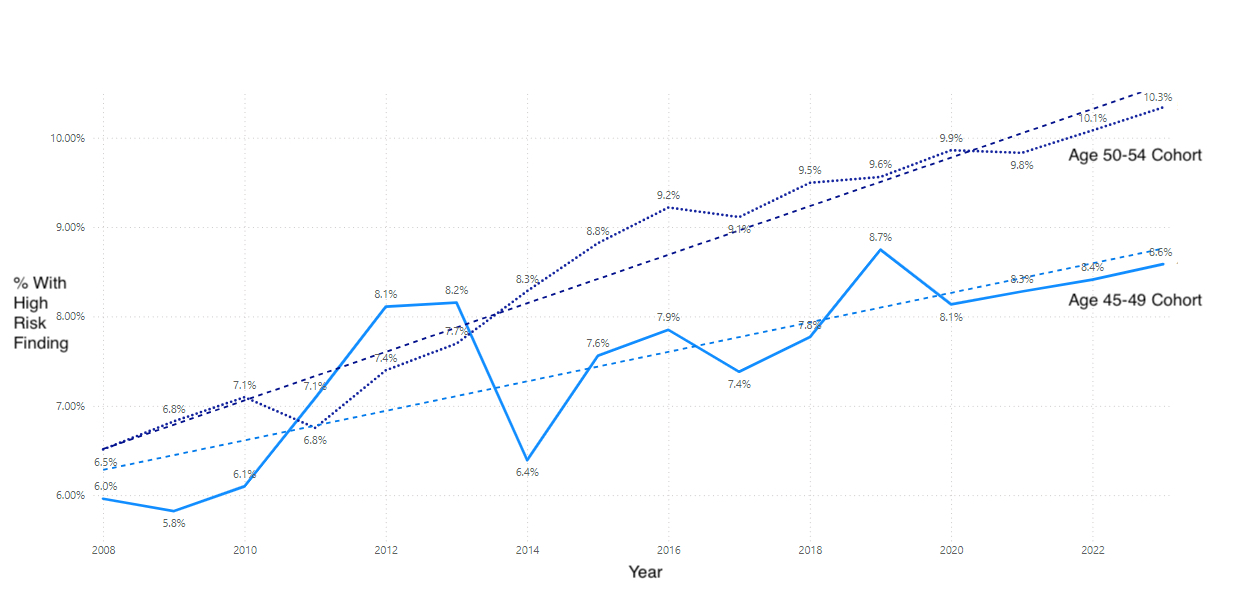
Figure: Trends in High Risk Findings Identified During Screening Colonoscopy
Disclosures:
Michael Smith: Castle Biosciences – Advisory Committee/Board Member, Consultant. CDx Diagnostics – Consultant. Lucid Diagnostics – Advisory Committee/Board Member, Consultant. Provation Medical – Consultant. Steris Endoscopy – Advisory Committee/Board Member, Consultant.
Stuart Amateau: Boston Scientific – Consultant. Cook – Consultant. Merit – Consultant. Olympus – Advisory Committee/Board Member. Provation – Advisory Committee/Board Member. Steris – Consultant.
Seth Gross: Cook – Consultant. Medtronic – Consultant. Microtech – Consultant. Olympis – Consultant. Provation – Consultant.
Nathan Merriman: Provation Medical – Advisory Committee/Board Member.
Steve Serrao: Provation Medical – Advisory Committee/Board Member.
Terry Bohlke: Provation Medical – Advisory Committee/Board Member.
Gregory Pepin: Provation Medical – Employee.
Carol Burke: Abbvie – Other. Ambry Genetics – Speakers Bureau. Emtora Biosciences – Grant/Research Support. Guardant – Consultant. Lumabridge – Consultant. Medtronic – Other. Myriad – Other. Sebela – Consultant.
Michael S.. Smith, MD, MBA1, Stuart K. Amateau, MD, PhD, FACG2, Seth Gross, MD3, Nathan A.. Merriman, MD, MSCE4, Steve Serrao, MD5, Terry Bohlke, 6, Gregory Pepin, 7, Carol A.. Burke, MD, FACG8. P0411 - Colorectal Cancer Screening in 45-49 and 50-54-Year-Olds Detects Similar Rates of High-Risk Findings: Results From a U.S.-Wide Cloud-Based Data Set, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
